Flu And Pneumonia Vaccines Are A Must
We say rheumatoid arthritis, you think joints which, of course, makes sense. Rheumatoid and other forms of inflammatory arthritis are notorious for causing pain, stiffness, and swelling in your hands, feet, lower back, and other joints.
But the same chronic, systemic inflammation that targets those joints can also affect other seemingly unrelated parts of your body such as your heart and your lungs.
Some reports suggest about 10 to 20 percent of patients with rheumatoid arthritis have lung problems. One study published in the journal Rheumatology International found that number may be as high as 67 percent. Most cases of lung disease will occur within five years of being diagnosed.
Scarring Within The Lungs
In medical speak, its called interstitial lung disease a broad category of lung disorders, most of which lead to scarring in the tissue between the air sacs of the lungs . Chronic inflammation from rheumatoid arthritis can lead to this scarring over time, the buildup of scar tissue makes the lung tissue stiff, which interferes with breathing and can be difficult to treat.
ILD is the most common and most serious lung complication for people with RA: Research shows lung disease alone accounts for up to 20 percent of deaths in rheumatoid arthritis patients, and most are attributed to ILD. Though its rare, this scarring may also occur in a small number of people with ankylosing spondylitis.
Symptoms include shortness of breath and dry cough, as well as fatigue and weight loss. But by the time these signs appear, irreversible lung damage has often already occurred. Some estimates suggest about 30 percent of patients with rheumatoid arthritis have ILD, without obvious symptoms.
When To Call Your Doctor
Seek medical care if you experience the following symptoms:
- Increased water retention with swelling of the legs, face, or hands
- Sudden shortness of breath
- Sudden fatigue or marked changes in energy levels
- Persistent or recurrent dizziness and lightheadedness
While these symptoms can be caused by any number of medical conditions, none should be considered normal. It is important to have them checked out.
On the other hand, you should seek immediate emergency care if you experience any of the following:
- Changes in the level of consciousness, including extreme sleepiness, difficulty waking up, or fainting
Recommended Reading: Rotary Bending Fatigue Testing Machine
Read Also: Fatigue Sore Muscles And Joints
Other Conditions That Cause Shortness Of Breath
Shortness of breath and other symptoms of anxiety can mimic other conditions. Its a good idea to monitor your symptoms and get a checkup with your doctor to rule out any other conditions.
Getting a physical to ensure you dont have any other issues can also alleviate some of your anxiety. For instance, in a panic attack, many people believe theyre having a heart attack. This fear only increases their panic.
Other causes of shortness of breath include:
Donât Miss: Why Does Colon Cancer Cause Fatigue
How To Help Keep Your Lungs Healthy
After heart disease, lung disease is the second-most common cause of death in rheumatoid arthritis. To help protect your lungs follow these three steps:
1. Quit smoking. Its harmful to your health in a million different ways. And the chemicals in cigarettes can irritate lung tissue even more. To get help, talk to your doctor or go to smokefree.gov. Quitting smoking can also help you achieve remission for your arthritis.
2. Get vaccinated. Respiratory infections are common infections in RA, and complications could be severe. There are two types of pneumonia vaccines talk to your doctor about which ones you need and when you should get them. The annual flu shot is another must. Heres what you need to know about getting the flu vaccine when you have arthritis.
3. Report any breathing problems to your doctor. Regular check-ups are important so your doctor can monitor your lungs. But be sure to tell your physician right away if you experience shortness of breath, consistent coughing, or other respiratory symptoms. Lung issues that are detected earlier may be easier to treat.
You May Like: What Can I Do For Extreme Fatigue
What Is Pots And Why Does It Cause Fatigue
POTS is a group of symptoms resulting from dysfunction of the autonomic nervous system. This branch of the nervous system regulates functions we dont consciously control like sweating and blood circulation.
In people with POTS, more blood collects in the lower body when standing upright. The heart beats faster to pump it up to the brain, but with little success. The causes of POTS are unknown, but the problem is thought to lie in the communication breakdown between the brain and the cardiovascular system.
POTS-related fatigue is physical in nature and the mechanism behind it is not fully understood. It may have several causes, including your body working harder to move the blood.
What Are The Types Of Lupus
There are three kinds of lupus:
- Systemic lupus erythematosus is the most common kind of lupus. It can affect many organs in the body.
- Cutaneous lupus usually affects only the skin with rashes on the scalp, legs, or arms.
- Drug-induced lupus happens as a reaction to some medicines. Symptoms usually go away when a person stops taking the medicine.
Recommended Reading: Plus Size Army Fatigue Joggers
Indirect Consequences Of Stress And Anxiety
The way we breathe is a powerful aspect of self-expression. Anxiety, emotional constipation, and other habits of mind and dysfunctional and self-limiting behavioural patterns might be associated with strong breathing patterns, especially shallow breathing.
Shallow breath is what we do when we literally hide . It is also what we do when we feel like we want to hide! Deep breathing is one of the main practical suggestions for fighting anxiety. Its a feedback loop.
Habitually breathing shallowly can be so subtle for so long that we dont even realize theres a problem until all the contributing factors and bad habits and vicious cycles are too deeply entrenched to break free a classic boiling frog kind of problem.
All of this is a rather complicated mess to try to sort out, but Im not going to leave you hanging. Here are several relevant, practical self-help articles. They all focus on what you can do about these issues:
Arthritis And Other Joint Problems
Several diseases and conditions can make your legs swell:
- Gout: A sudden painful attack caused by uric acid crystals in your joints that usually follows drinking heavily or eating rich foods. Learn more about the symptoms of gout.
- Knee bursitis: Inflammation in a bursa, a fluid-filled sac that acts as a cushion between bone and muscle, skin, or tendon. Learn how to treat knee bursitis.
- Osteoarthritis: The wear and tear type that erodes cartilage. Learn more about osteoarthritis symptoms.
- Rheumatoid arthritis: A disease where your immune system attacks tissues in your joints. Learn more about rheumatoid arthritis.
Read Also: Anti Fatigue Mats With Drainage Holes
You May Like: Anti Fatigue Mats For Hospitals
Cardiorespiratory Measurements During Exercise
Ventilation , oxygen uptake , carbon dioxide output , tidal volume , and respiratory frequency were measured breath by breath via a facemask. Heart rate was recorded using a Polar heart rate monitor linked directly to the metabolic system. ECG and arterial O2 saturation were monitored continuously using an ECG/pulse oximeter monitor . The CM5 ECG configuration was used to optimize the detection of any exercise-related rhythm disturbances.
Also Check: Vitamin D Deficiency And Fatigue
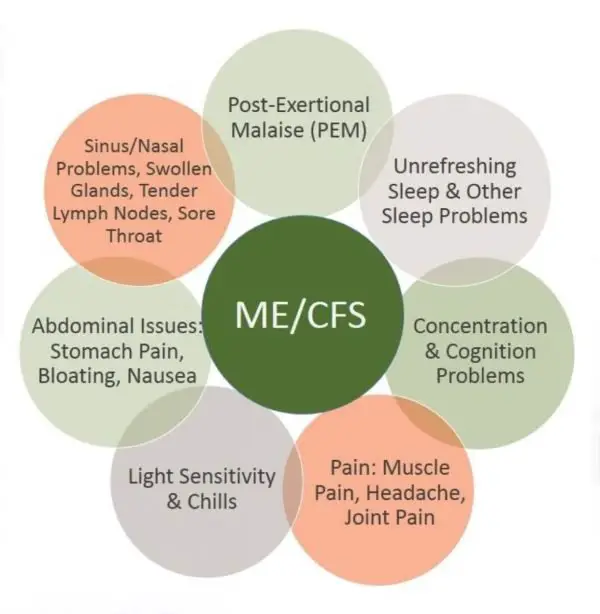
Pacing Activity For People With Me/cfs
Pacing, or keeping within your available energy, is a self-management strategy to help people with ME/CFS make sure that they dont overdo activity or exercise. It reduces the likelihood of triggering PEM and can help reduce symptoms. Pacing is not a cure for ME/CFS and does not treat the underlying, physical cause of the disease.
The goal of pacing is for activity to be sustainable, so that the person can have some stability in their symptoms and what they can do each day. Pacing should be used in conjunction with rest.
The most challenging aspect of pacing is that PEM is very often delayed by as much as 24-48 hours, which can make it difficult to recognise when youve done too much. Using tools like an activity diary or heart rate monitor help you learn about your body and how much activity you can safely tolerate.
Suggestions on how to pace yourself include:
Also Check: Hillside Anti Fatigue Kitchen Mat
What Should Someone Who’s Experiencing Post
For those who experienced only a mild illness and self-treated at home but are now dealing with post-COVID syndrome symptoms, Dr. Lahoti recommends scheduling an appointment with your primary care physician.
“Your doctor can diagnose the severity of your lingering symptoms, helping to treat the ones that are mild and referring you to a specialist for any that are more advanced,” explains Dr. Lahoti.
If you were hospitalized for more severe symptoms during your illness, you may already have a cardiologist you can follow up with about any heart issues, such as chest pain, or a pulmonologist you can check in with to address any lung issues, such as difficulty breathing.
“Because the symptoms of post-COVID syndrome are diverse and because this condition is so new and unique, we’ve created the Houston Methodist COVID-19 Recovery Clinic an entire clinic dedicated to helping people manage post-COVID syndrome,” Dr. Lahoti adds. “The purpose of this clinic is to bring together a range of specialists who have been on the front lines during this pandemic.”
The clinic will have a team of doctors specializing in:
- Physical Medicine & Rehabilitation
The clinic will also focus on performing impactful research, as well as providing doctors with access to tools that can help tailor care to the specific treatments someone previously received or the particular strain of the virus he or she was infected with.
Next Steps:
Other Areas Of Concern

- Ongoing joint pain or joint swelling is cause to see a rheumatologist for evaluation. Testing can show whether the problem is an inflammatory, auto-immune condition. The diagnosis is key to effective treatment.
- Persistent COVID-19 can trigger or worsen behavioral health problems. Doctors are seeing a range of problems from mild anxiety and health fears to extreme paranoia. Patients whose mental health is suffering due to COVID-19 are encouraged to get professional help.
You May Like: Can Back Pain Cause Fatigue
A Quick Success Story About Sore Breathing Muscles
I once developed a sharp pain in the side of my neck when I coughed or sneezed. It was clearly a muscular pain,12 specifically of the scalenes muscle group that kick in when you breathe hard. If I took a really deep breath, I could feel it a little too but it was mostly only clear when I coughed or sneezed.
Until I went for a run.
After a few minutes of huffing and puffing, that pain started up. I also felt distinctly short of breath, despite being generally quite fit. The pain was like a stitch in my side, but in my neck, and I was not getting full breaths. I realized I was barely using my diaphragm to breathe, and so my scalenes were working overtime to make up the difference and hurting and failing. I started using my diaphragm again and the pain steadily eased even though I kept running.
Not only was the pain clearly caused by over-using my scalenes while breathing, but I was able to fix a fairly significant pain problem without stopping my workout just by breathing differently. Thats a good, clear example of the easiest kind of breathing trouble to fix. What was going on?
How Is Chronic Fatigue Syndrome Diagnosed
Right now, theres no test to tell if someone has chronic fatigue syndrome. Doctors ask a lot of questions . They also will do a thorough physical exam.
Doctors also usually order blood, urine , or other tests to check for conditions that cause similar symptoms. They may send a person to see other specialists to help with the diagnosis.
A doctor may suggest meeting with a psychologist or a therapist who can see whether mental health disorders might contribute to or mask CFS.
Recommended Reading: Herbal Remedies For Adrenal Fatigue
Recommended Reading: Can Liver Disease Cause Fatigue
I: Trigger Pointsthe Effects Of Muscle Knots On Breathing
Trigger points better known as muscle knots can cause shortness of breath. They are small patches of sensitive muscle tissue, maybe caused by a micro cramp, or possibly neurological hypersensitivity. Trigger points are a big, tricky topic.
Trigger points may form in the muscles we use to breathe, making it difficult or even painful to move the ribs and expand the chest. Even the diaphragm itself might develop trigger points that make it feel weak and tired, and limit its range of contraction.8
Quick muscle knot orientation: So-called muscle knots AKA trigger points are small unexplained sore spots in muscle tissue associated with stiffness and soreness. No one doubts that they are there, but they are unexplained and controversial. They can be surprisingly intense, cause pain in confusing patterns, and they grow like weeds around other painful problems and injuries, but most healthcare professionals know little about them, so misdiagnosis is epidemic. For more information about how trigger points might be involved in your own medical history, see PainScience.coms popular e-book: The Complete Guide to Trigger Points & Myofascial Pain: An extremely detailed guide to the unfinished science of muscle pain, with reviews of every theory and treatment option.
Trigger points in the muscles of the throat, neck, chest, and back may also interfere with the nervous systems control of respiration.9
When To See A Healthcare Provider
If you’re worried you may be experiencing symptoms of an autoimmune condition, or if you have a strong family history of autoimmune disease, see your healthcare provider. They can give you a comprehensive evaluation and a physical exam to help provide a diagnosis.
Your doctor may also order blood tests such as:
- The antinuclear antibody test, which checks for specific antibodies to see if your immune system is attacking itself
- Complete blood count , which measures your blood cells
- Erythrocyte sedimentation rate, which checks for inflammation
If your healthcare provider thinks that you may have an autoimmune disease, you will likely be referred to a specialist. This might include a rheumatologist or an endocrinologist .
You May Like: Clinique For Men Super Energizer Anti-fatigue Depuffing Eye Gel
Is It Possible That I Have Pots And Was Incorrectly Diagnosed
This is entirely possible. Given how common POTS symptoms are and how unfamiliar many doctors are with this condition, diagnostic mishaps happen. POTS is frequently misidentified as chronic fatigue syndrome, fibromyalgia, myofascial pain syndrome, anxiety disorder, ADHD, irritable bowel syndrome, myositis, etc. It is also possible that you have both POTS and one of these conditions, which may complicate the diagnosis. Sometimes people with POTS are told that its all in your head, implying that the cause of their symptoms is psychological. If you feel like something is physically wrong, dont hesitate to seek a second, and even a third or fourth opinion.
COVID-19 and POTS: Is There a Link?
Although many people recover quickly from COVID-19, the disease caused by the coronavirus, others who recover may continue to experience symptoms for months. Researchers are still determining the cause of these extended symptoms, but some COVID-19 long-haulers may actually be dealing with POTS.
Nodules From Rheumatoid Arthritis In Lungs
These firm bumps of tissue, or rheumatoid nodules, might form in the lungs. They dont typically cause symptoms, nor do they pose a risk for lung cancer. Nodules range in size from a millimeter to centimeters in size, there may be one or a bunch, and they may come and go over time. In some cases, however, a nodule can rupture and caused a collapsed lung.
You May Like: Nicole Miller Anti Fatigue Floor Mat
A Cough Chest Pain And Shortness Of Breath
Shortness of breath is also a common symptom in patients with lung cancer, especially those with advanced stages of the disease.
Lung cancer patients often have shortness of breath, but also have a cough, chest discomfort, pain, or the sensation of heaviness, said Dr. Ronald Natale, medical director of the Lung Cancer Program.
As lung cancer develops, Dr. Natale says it can compromise breathing in 3 ways: The tumor can block airway passages, blood clots can form and block blood flow to an area of the lung, or fluid can build up in the lungs and chest wall causing the lungs to partially collapse.
A chest CT scan is usually the first step to investigate the cause of sudden-onset shortness of breath, says Dr. Natale.
Read: Should I Get a Lung Cancer Screening?
When Should I Call My Doctor About Pulmonary Hypertension
- Weight gain â 2 pounds in one day or 5 pounds in one week
- Swelling in your ankles, legs, or abdomen that has become worse
- Shortness of breath that has become worse, especially if you wake up short of breath
- Extreme fatigue or decreased tolerance for activity
- A respiratory infection or a cough that has become worse
- Fast heart rate
- Episodes of chest pain or discomfort with exertion that are not relieved with rest
- Difficulty breathing with regular activities or at rest
- Restlessness, confusion
Recommended Reading: Can High Blood Pressure Cause Fatigue
Is An Oxygen Level 94 Bad
It is essential to know what is normal for you in order to answer this question accurately. For some people, an oxygen level 96 is fantastic, while for others, an oxygen level 94 can be quite worrisome. The answer is entirely dependent on your overall health. An oxygen level 94 might be considered low for someone in average health, or it can be in the upper levels for someone living with COPD. If you are concerned about your oxygen saturation, talk to your doctor about what your normal O2 sat should be.