Reducing Alert Fatigue In Healthcare
Annoying.
That is the word that first comes to mind for many clinicians when they think about electronic health record alerts.
EHR alerts were originally designed to improve patient safety and medication accuracy. However, few clinicians would say thats the reality. Instead, most EHR users are inundated with constant reminders that are meant to be helpful but are really more of a nuisance.
The result is alert fatigue, where the constant bombardment of unhelpful data causes clinicians to disregard or fail to respond to warnings. Some doctors or nurses might see 100 to 200 alerts a day, said Amy Robbins, MD, one of the physician executives behind the PINC AI clinical decision support solution. While alerts can provide physicians with useful information and updates, many are unnecessary, such as alerts that tell clinicians things they already know.
Alert fatigue is not just an irritating distraction, it can also have serious consequences for patient care. For instance, alert fatigue can directly lead to burnout, which research shows can lead to medical errors and increased patient mortality.
PINC AIs CDS solution relies on natural language processing and machine learning to help health systems pinpoint the alerts that arent performing the way they should.
Ultimately, when it comes to CDS alerts, less is often more.
Amy Robbins, MD
Catrina Funk, MD, MBA
Data Collection And Analysis
In this section, we describe the planned methods for selecting studies and extracting and managing data. We also describe the means by which we will assess the quality of each study included in the review and how we will analyse and present the review findings.
Study selection
Search results will be entered into Mendeley Reference Management Software where duplicate entries will be removed automatically by an in built algorithm supported by manual checking.
Study selection will be undertaken by two reviewers independently.
Titles and abstracts will be screened with reference to the eligibility criteria to remove all ineligible articles. Translation of abstracts will be sought if required, prior to eligibility assessment. The full text of articles remaining will be sought and considered for inclusion in the review using the full eligibility criteria. Part translations of articles not in English will be undertaken to facilitate this process. Disagreements between reviewers will be resolved through discussion and with referral to a third reviewer if required. Articles excluded from the review at the full-text stage will be noted on the data extraction form as will the eligibility criteria these did not satisfy.
Critical appraisal, quality of reporting and data extraction
How One Hospital Tweaks Its Ehr To Fight Alert Fatigue
In Healthcare IT News‘ July cover story, which explores new and innovative approaches to clinical decision support at a time where it’s needed more than ever, one healthcare professional voiced a common complaint about electronic health records: the near-constant, often-annoying profusion of system alerts.
Too often, when clinicians think of CDS, “they think of a pop-up alert: something that, in the middle of what you’re doing, gives you a piece of information that the technology thinks is important and wants you to do something to fix,” said Gregory Paulson, deputy director of programs and operations at New Jersey-based Trenton Health Team.
But technology doesn’t always know best.
Paulson offered an analogy: “To me, it’s the equivalent of going online to shop on a website or pay your bill and getting these pop-up adds,” he says. “If you’re shopping on Amazon and you do it frequently, obviously you know where to click. You’re familiar with that website you know how to interface with it in a way that is seamless. So if I then institute a pop-up alert one that interrupts your process when you’re not expecting it and you don’t want to stop you’re not going to want to shop at Amazon.”
Same goes for physicians: The more they’re irritated by unneccesary alerts, the less they like using their EHRs.
At first, “we did the sledgehammer approach,” says Wes McMillan, UVMC’s clinical pharmacy manager.
You May Like: How To Combat Fatigue From Kidney Disease
Alert Fatigue Is An Alarming Problem
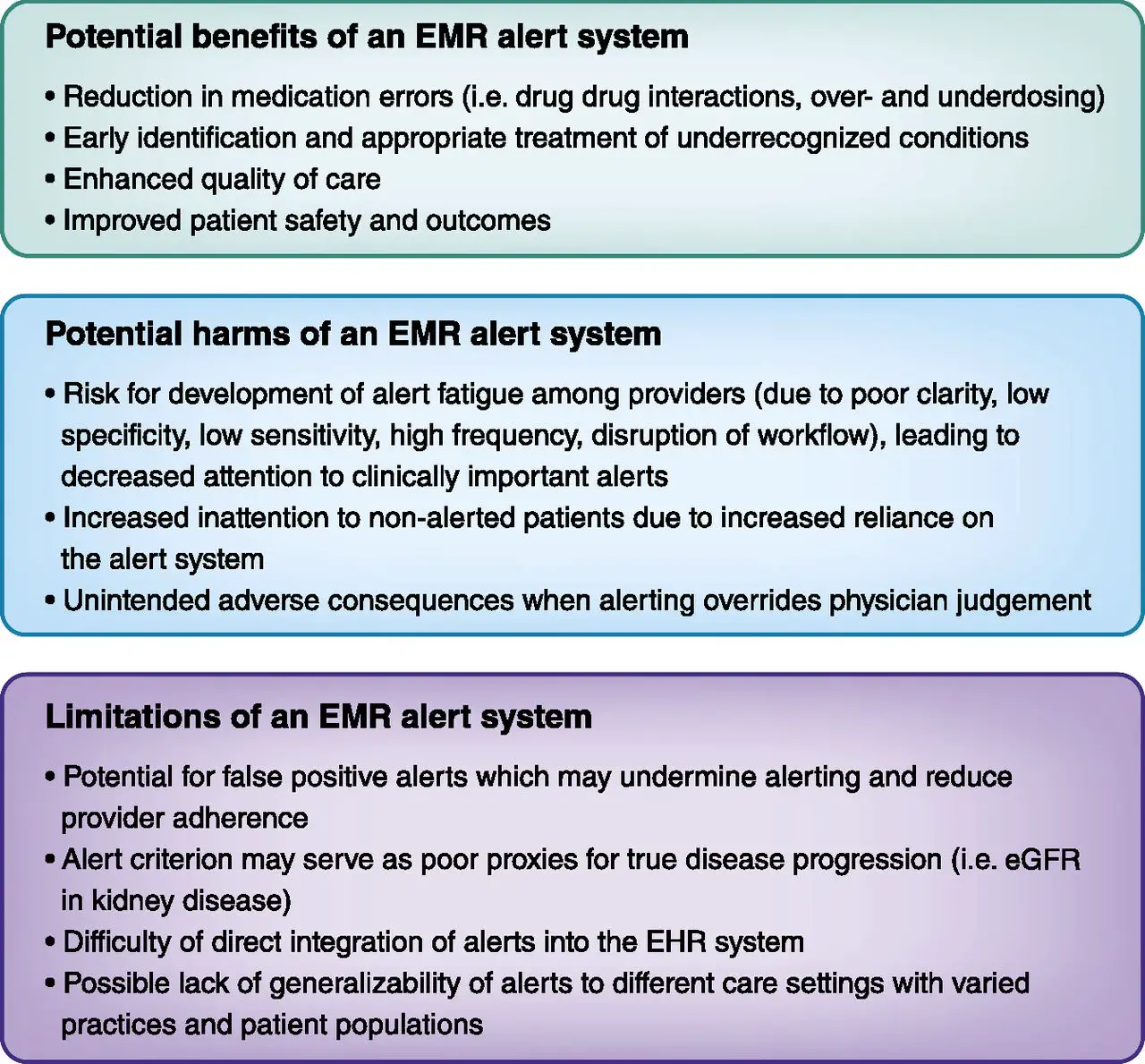
In theory, the more you alert a provider to potential problems, the better care the patient will receive. Of the many helpful features included within the framework of an electronic health record , provider pop-up alerts can simultaneously be one of the most positive and most negative depending on how theyre implemented. Too many alerts can lead to alert fatigue, which can be an alarming problem.
If implemented without proper alignment, alerts can have the inverse effect. When providers are inundated with pop-up messages, they focus less on the patient and their goal becomes getting out of the system instead of using the specified information to help the patient.
When an EHR is implemented for the first time, or an update is being installed that includes an increase in alerts, the IT or project team can feel that additional alerts inherently means increased patient safety. However, thats not necessarily the case. If alerts arent set up properly, they can downgrade patient care. Alert presentation and timing must be thoroughly vetted to ensure success.
A couple of things to keep in mind when setting up pop-up alerts:
- Alerts should provide ways to address issues or provide more information about issue, and
- Alerts should be integrated into the clinicians decision-making process.
Make sure to to our blog to get the latest in healthcare IT thought leadership, delivered right to your inbox.
Evaluating The Alert Appropriateness Of Clinical Decision Support Systems In Supporting Clinical Workflow
Review of critical issues on CDSS alert appropriateness and clinical workflow.
-
Appropriateness factors based on the Five Rights and socio-technical perspectives.
-
Proposed approach to evaluate appropriateness using Lean methods.
-
Recommended design of CDSS alert based on human automation and interaction concepts.
Don’t Miss: Chronic Fatigue Icd 10 Code
Alert Fatigue In Electronic Health Records
@article, author=, journal=, year=, volume=, pages=}
- Journal of the American Academy of Physician Assistants
- Australian prescriber
- Journal of medical Internet research
- Journal of oncology pharmacy practice : official publication of the International Society of Oncology Pharmacy Practitioners
Presentation Of Findings And Reporting Methods
The review will describe participant and setting characteristics, data collection and analysis methods. The findings of the primary papers will be summarised in tabular form describing the key characteristics of each. In addition, we will describe each paper narratively. The review findings will be classified into key themes as informed by the analysis. The reviews findings will also be summarised visually in a proposed conceptual framework explaining the relationship between the key factors influencing the efficacy of electronic alerts.
The protocol was developed and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis . The review methods and results will be reported according to the ENTREQ for reporting synthesis of qualitative studies . The final literature searches will be reported using the STARLITE .
You May Like: How To Beat Fibromyalgia Fatigue
Healthcare Organizations Across The Country Are Finding Creative Ways To Reduce Ehr Clinical Decision Alert Fatigue Through Optimization And Teamwork
May 13, 2021 – EHR alerts serve a significant purpose, but they can also result in EHR clinical decision alert fatigue, clinician burnout, or even frustration.
EHR alerts permit clinicians to access real-time patient data, ideally resulting in enhanced patient safety and medication accuracy. Alerts can also notify clinicians about potential adverse drug interactions.
According to Stanford University health IT professionals, EHR alerts are a vital part of EHRs that are not merely the use of technology it is using technology to find meaningful information to make clinical decisions and provide the best possible patient care.
Although a clinicians first instinct might be to close the alert to limit frustration, healthcare organizations attempt to limit alert quantity and improve alert quality to boost clinician satisfaction.
Data Analysis And Synthesis Of Results
We coded features and measurement methods as short descriptions . We sorted these descriptions into categories as commonalities emerged.
We also paid attention to the methods used to construct acceptance rates. In this article, we refer to the 2 main methods as in-dialog action analysis and event analysis.
In-dialog action analysis is only applicable when the CDS intervention takes the form of a dialog that features a button that the prescriber can click to modify or discard their order . Researchers count the number of times the acceptance button was clicked, and divide that count by the total number of dialogs that appeared.
Event analysis may be applied to any form of CDS, including dialogs. When conducting an event analysis, researchers search the patient chart for evidence that the prescriber accepted advice, in addition to any changes that prescribers may have made by clicking buttons inside CDS dialogs. For example, a prescriber might dismiss a modal dialog warning against a warfarin order, and then reduce the dose later. Or, a pharmacist might receive an alert from a CDS system, and counsel the prescriber by phonein which case the researchers must check to see if the prescriber made a change to the chart.
Next, we used a t test to compare acceptance rates between CDS systems by interactive design and clinical role-tailoring. In addition, we constructed a plot to holistically examine prescribers acceptance rates by feature.
Read Also: Joint Pain Back Pain Fatigue
Trends In Cds Interventions
Features present in 4 or more included studies are plotted cumulatively, over time, in . Three of the most common interactive featurestiering alerts, providing shortcuts for common corrective actions, and requiring a reason to overrideare described and illustrated in .
Feature prevalence over time. Pharmacists Received CDS is a subcategory of No Modals Interrupted Prescribers. All others are subcategories of Modals Interrupted Prescribers. CDS: clinical decision support.
The most commonly reported type of CDSwhich comprised 83% of resultsinterrupted prescribers with modal dialogs. The most common variants were tiered to convey levels of risk, provided shortcuts for common corrections, or required a reason to override.
We also found advisories that were not automatically issued using computerized systems. These included fax or mail alerts, and interactive designs in which a user manually retrieved a list of alerts or manually triggered a battery of modal dialogs. Only 1 article documented a design that allowed the user to dismiss a modal, and then retrieve it later for reference, rather than memorizing the contents of the alert. A list of all designs for presenting CDS is available in the Supplementary Appendix.
Optimizing Or Eradicating Low
Clinician burnout and EHR fatigue caused by alerts have been an issue for clinicians struggling with EHR usability overload.
READ MORE:The Pros and Cons of EHR Clinical Decision Support Alerts
Although EHR alerts can offer providers practical suggestions and updates, EHR alert fatigue has been an issue for clinicians already struggling with EHR usability problems. Low-value EHR alerts can disrupt patient care and contribute to clinician burnout.
At Brigham and Womens Hospital, clinicians were getting roughly one alert for every two medication orders, and clinicians were overriding an astounding 98 percent of the alerts.
One of the big issues is that many of the clinical systems that are in routine use today, alert too frequently, David Bates, MD, chief of the Division of General Internal Medicine at Brigham and Womens Hospital, said in an interview with EHRIntelligence. When clinicians are overriding that high a proportion of alerts, clinicians get very used to closing the alert, and sometimes they arent fully processing what the alerts are saying and they tend to stop paying attention to the important alerts.
Unsatisfied with how their EHR vendor fired off alerts, Bates and his health IT team tapped Seegnal eHealth to leverage its EHR alert solution and conduct an EHR alert study at the hospital.
READ MORE:The Deadly Consequences of EHR Clinical Decision Support Tools
READ MORE:5 Ways to Improve CDS Tools, Minimize Clinician Burden
You May Like: How To Beat Crohn’s Fatigue
Effect Of Alert Fatigue On Patient Safety
Much of the literature on alert fatigue derives from studies of CPOE and clinical decision support systems, in which alerts are provided to warn of potentially harmful drugdrug interactions or incorrect medication doses. These studies consistently show three main findings:
- Alerts are only modestly effective at best. A systematic review of computerized reminders found only minor improvements in targeted processes of care, and, while CPOE systems have been shown to prescribing errors, this can largely be ascribed to their ability to standardize drug doses, provide decision support, and eliminate errors from poor handwriting or incorrect transcriptions.
- Alert fatigue is common. Clinicians generally override the vast majority of CPOE warnings, even “critical” alerts that warn of potentially severe harm. There is less literature on other types of warnings, but it is likely that rates of overriding or ignoring warnings in other settings are also high.
- Alert fatigue increases with growing exposure to alerts and heavier use of CPOE systems. This finding is intuitive, but also raises the important implication that without system redesign, the safety consequences of alert fatigue will likely become more serious over time.
Alert Fatigue: Refining Accuracy To Reduce Burden

Todays healthcare technologies help streamline workflows, improve the patient experience, and manage the quality and cost of care. However, despite recent improvements, Electronic Health Records , Clinical Decision Support , and similar systems are still lacking in some areas. For example, conventional systems are commonly known to send irrelevant alerts, which are disruptive and often provide little assistance. Nearly 70% primary care providers report these alerts are unmanageable.
High alert volume, coupled with low clinical relevance, has led many clinicians to alert fatiguea scenario in which clinicians receive so many clinically irrelevant alerts that they become desensitized to all alerts, regardless of their relevance and value. As a result, clinicians lose trust in the alerts and may fail to acknowledge the appropriate ones, perpetuating this vicious cycle and putting themselves and their patients at risk.
Also Check: Vitamin D Deficiency And Fatigue
What Are The Goals Of The Group
Every time we meet or think about CDS, we always focus on our driving philosophy of the five rights. Our mission is to ensure the right information goes to the right person at the right time, in the right place, format and channel. And we apply that philosophy to three buckets:
1. Review requests to build new alerts.
One of the first things we did was overhaul and standardize our intake process. The objective of this committee was to challenge requestors from the start to be thoughtful with what theyre trying to solve. We wanted to understand if there was a larger safety or security event behind the request, the scope of the impact and how they were going to measure the success of the functionality. From there, we would examine if the rationale made sense. We also checked if there were alternate, less-intrusive CDS tools to consider, that might be a better fit for the workflow. As a result of this new process, we were able to ensure the consistency of alerts across the enterprise to help guarantee that patients receive the same expert level of care, regardless of what location and specialty they visited.
2. Review legacy alerts for relevance and efficacy, then deactivate or update accordingly.
3. Review recently approved alerts and make sure theyre accomplishing their stated intention.
The Problem Of Alert Saturation
Whenever new technology is implemented for the first time, it is not uncommon for problems that crop up that require adjustments by the user. Many times this includes customizing the technology in its responses to best serve the users interests. A particular problem faced by EHR users is referred to as alert fatigue. This occurs when medical personnel are continuously subjected to alert pop-ups as they work the electronic medical records system.
Theoretically, the more alerts a medical provider receives about a patient or particular treatment, the better care they can provide the patient. However, these alerts can work against this theory and result in negative consequences for patients if the technology is not adjusted and customized properly. An excessive amount of alerts, many of which are already known by the medical provider, can lead to alert fatigue.
When medical personnel are saturated with these pop-up messages, they may remove some of their focus from the patient and toward eliminating the nuisance of the unnecessary pop-ups. This can also lead to a situation where an important alert is missed by the healthcare provider, leading to potentially dangerous results for the patient.
Generally, less is more when it comes to EHR alerts. A gradual and balanced implementation of new alerts is best at the outset. Testing of the alert system on the backend is very important to ensure they are firing with the correct information and at only the necessary times.
Recommended Reading: What Is The Cure For Chronic Fatigue Syndrome
Ereferral Acceptability And Staff
In addition to providing ratings, 106 of the 113 post-implementation survey respondents completed open-ended survey questions about their perceptions of WTQL referral facilitators and barriers. Many responses identified lack of time or time pressure as a barrier to addressing tobacco use well. One respondent wrote With everything else that is being thrown at primary care, I find I have less and less time to address even important things like smoking cessation at office visits. Another described the following barrier: Increasing demands on time in regard to satisfying electronic medical records and organizational requirements for best practice protocol. This results in much less time with patients and much more time in front of the computer.
In addition, consistent with stakeholder input before and during implementation , many clinic staff in eReferral clinics noted that task sharing and workflows could be improved by using a team approach or having nurses provide cessation counseling and education. Some nurses noted, though, that inadequate communication with clinicians and insufficient clinician support and trust for nurses or medical assistants to offer smoking treatment were barriers to tobacco treatment. Some reported, too, that patients want to receive quitting advice from their physicians.