This Page Has Been Archived
Information identified as archived is provided for reference, research or record-keeping purposes. It is not subject to the Government of Canada Web Standards and has not been altered or updated since it was archived
Chronic Fatigue Syndrome , also known as Myalgic Encephalomyelitis , is a debilitating and potentially disabling illnessFootnote 1-7 that affects over half a million Canadians Footnote * .Footnote 8 CFS/ME is not yet fully understood, but it is known to affect multiple systems of the body. Footnote 1-7
What Is Chronic Fatigue Syndrome
Chronic fatigue syndrome is a complicated disease for doctors to diagnose and even fully understand.
CFS is a chronic condition that makes people feel very tired and weak. They can also have headaches, dizziness, or other physical symptoms. Sometimes they have emotional symptoms too, like anger or sadness.
Different people with CFS can have different symptoms. Many CFS symptoms are similar to those of other health conditions, like mono, Lyme disease, or depression. And the symptoms can vary over time, even in the same person.
This makes treating the illness complicated. No single medicine or treatment can address all the possible symptoms.
CFS is sometimes called myalgic encephalomyelitis . Myalgic means muscle aches. Encephalomyelitis means that there may be inflammation in the brain or spinal cord.
How Is Chronic Fatigue Syndrome Diagnosed
CFS diagnosis depends on two criteria:
A specific treatment for CFS has yet to be proven effective. Vitamin supplements and medicines have some benefit. Many treatments just relieve the symptoms of CFS.
Read Also: Constant Fatigue And Body Aches
What Are The Signs & Symptoms Of Chronic Fatigue Syndrome
Someone with chronic fatigue syndrome can have many possible symptoms. The most common ones include:
- severe fatigue, which can make it hard to get out of bed and do normal daily activities
- sleep problems, such as trouble falling or staying asleep, or not having a refreshing sleep
- symptoms getting worse after physical or mental effort
- symptoms or dizziness that get worse after standing up or sitting upright from a lying down position
- problems with concentration and memory
- headaches and stomachaches
Assessment And Treatment Of Me/cfs Patients:
Also Check: Best Books On Adrenal Fatigue
Diagnosis And Treatment For Me/cfs
Currently, there is no single test to diagnose ME/CFS. Doctors make a diagnosis by excluding all other illnesses that might be causing symptoms and following accepted diagnostic criteria. The persons results from routine medical tests will often be normal, but additional tests may show abnormalities.
How Does Me/cfs Affect People
ME/CFS affects different people in different ways, some more severely than others. There are four levels of severity of ME/CFS, which give an indication of the level of disability ME/CFS can create:
- mild: 50% reduction in pre-illness activity
- moderate: mostly housebound
- severe: mostly bedridden
- very severe: totally bedridden and need help with basic activities including nutrition and hydration.
The severity of ME/CFS can vary over time. A person living with ME/CFS could be at one level of severity now, then their disease could either improve or deteriorate over time. For some patients, their disease can worsen significantly with no known cause. Other patients have a fluctuating illness where they have better and worse periods, which last for months or years. It is unclear why this happens.
For most people, ME/CFS is a lifelong disease. Full recovery is rare and estimated at less than 10%. For some people with ME/CFS, as time passes and their disease improves, they will find they can do more, but it is a slow and gradual process. However, this is not the case for everyone. Some people find their disease worsens over time, others may remain somewhat stable. With support and pacing, people can often improve their quality of life.
Don’t Miss: Hypersomnia Vs Chronic Fatigue Syndrome
Long Covid/ Long Haulers
Following the outbreak of COVID-19 in late 2019 in Wuhan Province, China, and its rapid spread into other parts of the world, researchers, scientists, and patients familiar with post-viral syndromes began to become concerned not only about the acute danger of this particular virus but the potential long-term sequelae. Following SARS-1, West Nile Virus, H1N1 influenza virus, and other reports claim, that up to 11% of patients who had severe infections from Epstein-Barr virus , Q fever , or Ross River virus , and others, develop ME/CFS. Other studies following SARS and MERS suggest an even higher proportion develop ME/CFS or Fibromyalgia.”
Given that some estimates suggest as much as 75% of all ME/CFS patients developed their illness following a post-viral or post-bacterial illness, there has been considerable frustration in the ME/CFS community-researchers and patients alike-that had ME/CFS patients been taken more seriously all along, then research into what causes this debilitating outcome in some patients and not in others would have been identified and potentially remedied by now.
Additionally, there is great frustration in the ME/CFS community as they watch these new cases as they are now being officially diagnosed as they pass the six-month mark required for official ME/CFS diagnosis.
The Role Of Neuroglia In Brain Function And Central Nervous System Inflammation
Neuroglia in the CNS consist of heterogeneous cell populations: microglia, astrocytes, oligodendrocytes and ependymal cells. Astrocytes are neural cells of ectodermal origin that are the predominant glial cells in the brain, whereas microglia are long-lived innate immune cells of mesodermal origin. Oligodendrocytes and their progenitor cells are mainly involved in providing axonal insulation and myelination, which proceeds throughout life . Microglia, astrocytes, and oligodendrocytes interact both with neurons and with each other via signaling molecules, and form long-range networks supporting and regulating the neuronal connectome . Thus, they are key elements of CNS homoeostasis and protection, and in some respects interact to a degree where they can be considered one dynamic functional unit.
Possible pathobiological mechanisms whereby neuroglia may become reactive in ME/CFS. Note the possible contribution of immune processes , metabolic dysfunction, endothelial/vascular dysfunction and oxidative/nitrosative stress.
Recommended Reading: Shortness Of Breath Chest Pain Fatigue
Chronic Fatigue Syndrome Symptoms
The onset of chronic fatigue syndrome symptoms can be fairly sudden , or more gradual. Chronic fatigue syndrome should be suspected if the following symptoms are not explained by any other condition, and persist for a minimum of six weeks in adults, or four weeks in children and young people:
- Extreme tiredness that is worsened by activity, but is not caused by excessive exertion, and is not significantly relieved by rest.
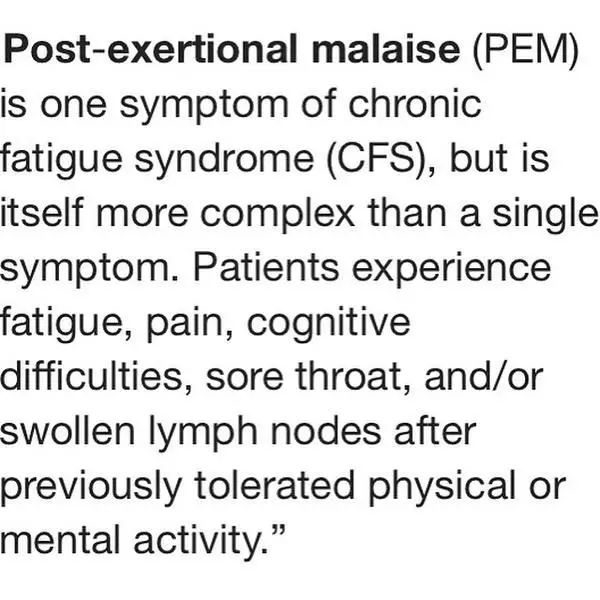
- Post-exertional malaise : feeling unwell with no energy after activities, with a worsening of symptoms that:
- Often doesn’t start until hours or days after the activity.
- Is much greater that you would expect for that particular activity.
- Has a prolonged recovery time that may last hours, days, weeks or longer.
- Difficulty concentrating or multitasking.
- Inability to engage fully in work, educational, social or personal activities is a common symptom.
The diagnosis can only be confirmed after three months of persistent long-term symptoms, but only if the symptoms cannot be explained by any other condition.
Graded Exercise Therapy Controversy
The PACE TRIAL
In 2005, patient recruitment began for the PACE Trial – Pacing, Graded Activity, Cognitive Behavioral Therapy, and randomized Evaluation, which was conducted in the UK under the auspices of the UK Medical Research Council, Depart of Health and Social Care for England, Scottish Chief Scientist Office, and Department for Work and Pensions. The investigators were Peter White, a psychiatrist, Trudie Chalder, a professor of cognitive behavioral therapy, and Michael Sharpe, a professor of psychological medicine.
This study, which is the most well-funded single piece of ME/CFS research ever conducted, was designed to compare three different approaches to treatment:
1) Specialist Medical Care , which included the use of medications for symptoms management and instruction in avoidance of extreme activity or inactivity to SMC plus Adaptive Pacing Therapy , which is activity engagement limited by symptoms of PEM on one extreme and complete inactivity on the other
2) Informing the group that they were not ill, but rather deconditioned and should gradually return to activities and that there was nothing preventing their recovery and
3) CBT and GET with the premise that deconditioning, dysfunctional cognition, and false ideas were the source of their symptoms and functional limitations. The GET was to be advanced in a structured manner with the ultimate goal of the patients participating in regular aerobic exercise.
The consequences of the PACE Trial were:
Read Also: What Is Rheumatoid Arthritis Fatigue
Caring For Someone With Me/cfs
Having a supportive community of family, friends, school, work, employers and health workers, who understand the potential seriousness of ME/CFS, can also help improve the quality of life of people living with ME/CFS.
Everyone involved in supporting someone with ME/CFS needs to understand Post Exertional Malaise, which is an abnormal, biological response to exercise or activity. This means the patient will not be able to do all of the activities they used to be able to do, and will benefit from practical and emotional support. People with ME/CFS will each have different needs and preferences, so it is important to talk with them about how best to provide support. This may include help with daily routines, family life, accessing healthcare and other personal priorities.
Problems With Thinking Memory And Concentration
If you have ME/CFS, it’s also common to have:
- problems remembering certain words, names or numbers
- difficulty concentrating or difficulty focusing on more than one thing at a time
- problems remembering things that happened recently
- being slow to speak or react to things
These problems are sometimes described “brain fog”.
Read Also: Tough Guy Anti Fatigue Mats
Not All Forms Of Neuroglial Dysfunction May Be Neuroinflammation
Does the involvement of neuroglia necessarily point to neuroinflammation? As we have seen, the answer is yes and no, and here we touch on the ongoing discussion about the definition of CNS inflammation and the role of glia in the CNS. Most basically, microglia can be understood as the central part of the innate immune system of the CNS. Neuroglial reactivity, therefore, may indeed be associated with or reflect inflammatory changes in the CNS or mirror inflammation outside the CNS. Inflammation constitutes defensive activity of the innate immune system, whether peripheral or central, to various types of insults including stress. This response can be beneficial or detrimental depending on the context and magnitude, and typically involves the release of cytokines, and increased phagocytic activity. Such activity can be directed toward pathogens, but also toward stressed neurons and synapses .
Abnormal Cerebral Blood Flow
Indirect evidence of dynamically abnormal regional CBF comes from the consistent finding in ME/CFS patients that wider regions with greater blood oxygenation are activated in response to different tasks . The latter has been interpreted as an indication of disrupted NVC .
In a recent MRI study of 31 ME/CSF patients using a pseudo-continuous arterial spin labeling technique, significant regional CBF abnormalities in several brain regions of the limbic system were noted at rest, i.e., without orthostatic or exercise challenge . The assumption of regional CBF abnormalities may be further supported by structural MRI findings of regional white matter loss in the left inferior fronto-occipital fasciculus and in the brain stem , sites that are particularly sensitive to hypoxia. So far the most salient imaging evidence for abnormal CBF in ME/CFS arises from findings of a paradoxical reorganization of local blood flow in the anterior node of the DMN after physical exercise .
Clearly, impaired CBF appears so central in ME/CFS that any hypothesis on the pathobiological underpinning of ME/CFS needs to account thereof. Physiologically, how well oxygen and nutrients are delivered to brain cells depends on adequate blood flow to the brain, competent vascular autoregulation, adequate NVC as well as local microvascular competence. Several hypotheses, that are not mutually exclusive, have been put forth on how the blood flow may be altered in ME/CFS.
Recommended Reading: How To Explain Ms Fatigue
Professional Values And Support For People With Cfs/me And Their Families
Specialist HCPs identified a core minority group of GPs in their region who made referrals to their service, but contrasted these GPs with the many who did not understand CFS/ME, and who see it as a psychological rather than a physical condition. They reported whole practices as having decided that CFS/ME did not exist and that many GPs would never make a referral to a specialist service. Participant HCPs reported how some patients told them that their GP openly stated their lack of belief in the existence of CFS/ME.
All participants emphasised the importance and powerful therapeutic value of listening. One specialist said that, “patients will often say ‘you’re the first people that have actually listened to me'” . Time limits in the primary care system often constrain patients from recounting their full story, and, “the doctor is too busy, they don’t have time really facing the patients for five minutes just to say OK, then the computer, then done” . However, these participants reiterated the need for practitioners to be knowledgeable, empathic, inventive and capable of learning, acknowledging the patient’s condition and taking it seriously. They should be able to respond flexibly to people’s needs, accommodate the difficulties inherent in the condition that affect concentration and/or physical access, remain positive and encouraging and work in ways that engender a trusting relationship.
The Concept Of Neuroinflammation Or Central Nervous System Inflammation
Lately, the investigation of inflammatory processes in the CNS has received increased attention in ME/CFS research . The concept of CNS inflammation is still being conceptualized in detail and commonly refers to inflammatory processes taking place in the CNS to counteract infection, eliminate cellular debris or generally protect the integrity of the CNS. As an essential component of the innate immune repertoire of the CNS, this inflammation is typically mediated by the resident immune cells of the CNS, microglia, in concert with astrocytes, microvascular endothelial cells and peripheral immune cells that can migrate into the CNS. Inflammation in the CNS sets off a well-orchestrated response, which includes the release of inflammatory mediators and activation of downstream signaling pathways that can disrupt the blood-brain barrier , thus increasing perfusion and facilitating immigration of blood immune cells. The inflammatory response can also exacerbate or induce cellular stress, mitochondrial dysfunction, myelination defects and synaptic loss .
On the functional level, CNS inflammation has been associated with cytokine-mediated sickness behavior , excitotoxicity and dysfunctional connectivity within the brain that leads to CNS dysfunction affecting sleep, circadian rhythm, emotional processing, cognition, learning and memory, pain, and autonomous regulation.
Recommended Reading: Can Kidney Stones Cause Fatigue
Other Chronic Fatigue Syndrome Symptoms
Other symptoms that may be associated with CFS/ME include:
- Dizziness, palpitations, fainting, nausea on standing or sitting upright from a lying position.
- Increased sensitivity to temperature, causing increased sweating, chills, hot flushes or feeling very cold.
- Twitching and other abnormal uncontrolled body movements.
- Flu-like symptoms, including sore throat, tender glands, nausea, chills or muscle aches.
- Intolerance to alcohol, or to certain foods or chemicals.
- Increased sensitivities, including to light, sound, touch, taste and smell.
- Pain, including pain on touch, muscle pain, headaches, eye pain, tummy pain, or joint pain.
What Are The 3 Types Of Fatigue
There are three types of fatigue: transient, cumulative, and circadian:
- Transient fatigue is acute fatigue brought on by extreme sleep restriction or extended hours awake within 1 or 2 days.
- Cumulative fatigue is fatigue brought on by repeated mild sleep restriction or extended hours awake across a series of days.
Don’t Miss: How Do I Know If I Have Chronic Fatigue Syndrome
Is Fibromyalgia A Disability Uk 2021
In the UK, a person is considered disabled if they have a physical or mental impairment that has a ‘substantial’ and ‘long-term’ negative effect on their ability to do normal daily activities. The Department for Work and Pensions recognises fibromyalgia as a real and potentially significantly disabling condition.
Guidelines For Diagnosing Me/cfs

Guidelines from the National Institute for Health and Care Excellence say doctors should consider diagnosing ME/CFS if a patient has extreme tiredness that cannot be explained by other causes and the tiredness:
- started recently, has lasted a long time, or keeps coming back
- means you cannot do the things you used to do
- gets worse after activity or gentle exercise, such as a short walk
You must also have some of these symptoms:
- problems sleeping, such as insomnia
- muscle or joint pain
- fast or irregular heartbeats
- doing exercise or concentrating makes your symptoms worse
The GP should consult a specialist if they’re unsure about the diagnosis or if you have severe symptoms.
If a child or young person under 18 has symptoms of possible ME/CFS, they may be referred to a paediatrician.
As the symptoms of ME/CFS are similar to those of many common illnesses that usually get better on their own, a diagnosis of ME/CFS may be considered if you do not get better as quickly as expected.
The diagnosis should be confirmed by a doctor after other conditions have been ruled out, and if your symptoms have lasted at least 3 months.
Page last reviewed: 29 October 2021 Next review due: 29 October 2024
Don’t Miss: Best Shoes For Foot Fatigue