Redox Imbalance Links Covid
See allHide authors and affiliations
General Exercise Tips For People With Chronic Fatigue Syndrome
Be guided by your doctor or specialist, but general suggestions include:
- Experiment to find the type of exercise that works best for you. Choose from a range of gentle activities such as stretching, yoga, tai chi, walking and light weight training.
- Keep an activity diary so you have a long-term picture of your performance levels and factors that might impact on your symptoms.
- Stop the physical activity well before you feel any symptom flare. Pacing yourself is very important.
- Remember that the amount of exercise you can do will change from one day to the next.
- Listen to your body if you dont feel up to exercising on a particular day, dont.
- Find out as much as you can about your ME/CFS. Make sure you consult with health professionals who fully understand ME/CFS as a ‘real’ biomedical condition.
Impaired Energy Metabolism In Me/cfs
Metabolomic studies have reported evidence of impaired ATP production from oxygen, glucose, fatty acids, and amino acids in multiple cell types . Not just oxidative phosphorylation but also glycolysisand possibly, the citric acid and urea cyclesare incriminated. In people with ME/CFS, there also is a more general hypometabolic state as previously proposed , characterized by depressed levels of most metabolites, as occurs in hibernating animals . Later, we speculate as to the cause of this hypometabolic state.
Both structural and functional mitochondrial abnormalities have been found in ME/CFS. Branching and fusion of mitochondrial cristae are observed in muscle biopsies of some patients . Although some studies have reported deletions of mtDNA genes, the most extensive controlled study using contemporary technology did not find mtDNA variants that correlated with susceptibility to ME/CFSalthough it did find a correlation between specific haplogroups and mtDNA single-nucleotide polymorphisms and specific symptoms . Other reports have identified a deficit in Complex V activity of the electron transport chain in lymphocytes, with a compensatory up-regulation of respiratory capacity , and a decrease in mitochondrial membrane potential in CD8+ T cells . Serum from ME/CFS patients reportedly contains a factor that induces mitochondrial fragmentation .
Don’t Miss: How To Combat Chronic Fatigue
Interaction Between Herpesvirus Infection Status And Lymphocyte Phenotype And Function
Herpesvirus infection, most notably infection with CMV, is known to affect both the maturational phenotype and the function of human CD8+ T cells and NK cells . We therefore compared lymphocyte phenotype and function among those subjects who were either seropositive or not for CMV. Across all the study groups, participants who were CMV-seropositive had significantly lower proportions of CD4+ and higher proportions of CD8+ T cells amongst their PBMC . Following stimulation with PMA and ionomycin, higher proportions of both CD4+ and CD8+ T cells made IFN, and more cells were IL-2 and IFN double positive, amongst CMV seropositive individuals. The proportion of PBMC which were CD3+CD56+ cells was highly significantly enhanced amongst CMV-positive participants. In the NK cell population, more cells were NKG2C+, and there were decreased proportions of CD56dimCD57intermediate and increased proportions of CD56dimCD57bright amongst CMV-seropositive participants. Amongst CMV-seropositive individuals, there was a decreased in vitro response to IL-12 and IL-18 stimulation, with significantly reduced CD25, CD107, and IFN expression .
World Chronic Fatigue And Immune Dysfunction Syndrome Day
12 May
This day is used to make the public aware of what Chronic Fatigue and Immune Dysfunction Syndrome is about.
Chronic fatigue syndrome is more than just fatigue. It is a serious, debilitating medical condition. Individuals with CDS experience various problems including pain in the muscles and joints, tender lymph nodes, headaches, prolonged, extreme exhaustion following physical or mental activity and many other symptoms.
CFS is a real medical condition. There is no known cause or cure for CFS, but scientists have identified numerous biological abnormalities in CFS patients. CFS is not psychological in origin. Medical studies have proven CFS is not all in the head, laziness or a mental disorder.
CFS can be treated. Physicians can help improve a patients quality of life by treating symptoms such as sleep disorders, pain and gastrointestinal difficulties.
Related links
Don’t Miss: Vitamins For Adrenal Fatigue Syndrome
How Is Chronic Fatigue Syndrome Diagnosed
CFS can be difficult to diagnose. There is no specific test for CFS, and other illnesses can cause similar symptoms. Your health care provider has to rule out other diseases before making a diagnosis of CFS. He or she will do a thorough medical exam, including:
- Asking about your medical history and your family’s medical history
- Asking about your current illness, including your symptoms. Your doctor will want to know how often you have symptoms, how bad they are, how long they have lasted, and how they affect your life.
- A thorough physical and mental status exam
- Blood, urine, or other tests
Background And Main Text
Myalgic encephalomyelitis/chronic fatigue syndrome is a complex and controversial clinical condition without having established causative factors. Increasing numbers of cases during past decade have created awareness among patients as well as healthcare professionals. Chronic viral infection as a cause of ME/CFS has long been debated. However, lack of large studies involving well-designed patient groups and validated experimental set ups have hindered our knowledge about this disease. Moreover, recent developments regarding molecular mechanism of pathogenesis of various infectious agents cast doubts over validity of several of the past studies.
Read Also: Does Strep Throat Cause Fatigue
Chronic Fatigue Syndrome: New Evidence Of Immune Role
Researchers recently investigated the immune systems role in chronic fatigue syndrome in unprecedented depth. The findings might help design future treatments.
Chronic fatigue syndrome , or myalgic encephalomyelitis , is a mysterious condition.
The main symptom of CFS is extreme and often unrelenting fatigue. Others include muscle and joint pain, sleep issues, and flu-like symptoms.
Researchers do not yet know what causes CFS. Suggestions include viral or bacterial infection, changes in the immune system, hormone imbalance, and mental health conditions.
Because of this, they have not yet been able to design a test that can diagnose CFS, and current treatments only relieve symptoms.
Over the years, interest in the role that the immune system might play in CFS has grown.
Often, people with CFS report that their symptoms began following an infection or other insult to the immune system. These reports are common, but once symptoms have appeared, it is impossible to assess how the body was behaving before they arrived.
Researchers from the Institute of Psychiatry, Psychology, and Neuroscience at Kings College London in the United Kingdom used an interesting model to delve deeper.
The researchers investigated people who were taking a treatment for hepatitis C called interferon-alpha. Interferon-alpha works by triggering the immune system in the same way that a significant infection would.
Some Of The Areas That Are Being Studied As Possible Causes Of Me/cfs Are:
People with ME/CFS often have their illness begin in a way that reminds them of getting the flu. This has made researchers suspect an infection may trigger ME/CFS. In addition, about one in ten people who become infected with Epstein-Barr virus, Ross River virus, or Coxiella burnetti will develop a set of symptoms that meet the criteria for ME/CFS. People with these infections who had severe symptoms are more likely than those with mild symptoms to later develop ME/CFS symptoms. But not all people with ME/CFS have had these infections.
Other infections that have been studied in connection with ME/CFS are human herpesvirus 6, enterovirus, rubella, Candida albicans, bornaviruses, mycoplasma, and human immunodeficiency virus . However, these infections have not been found to cause ME/CFS.
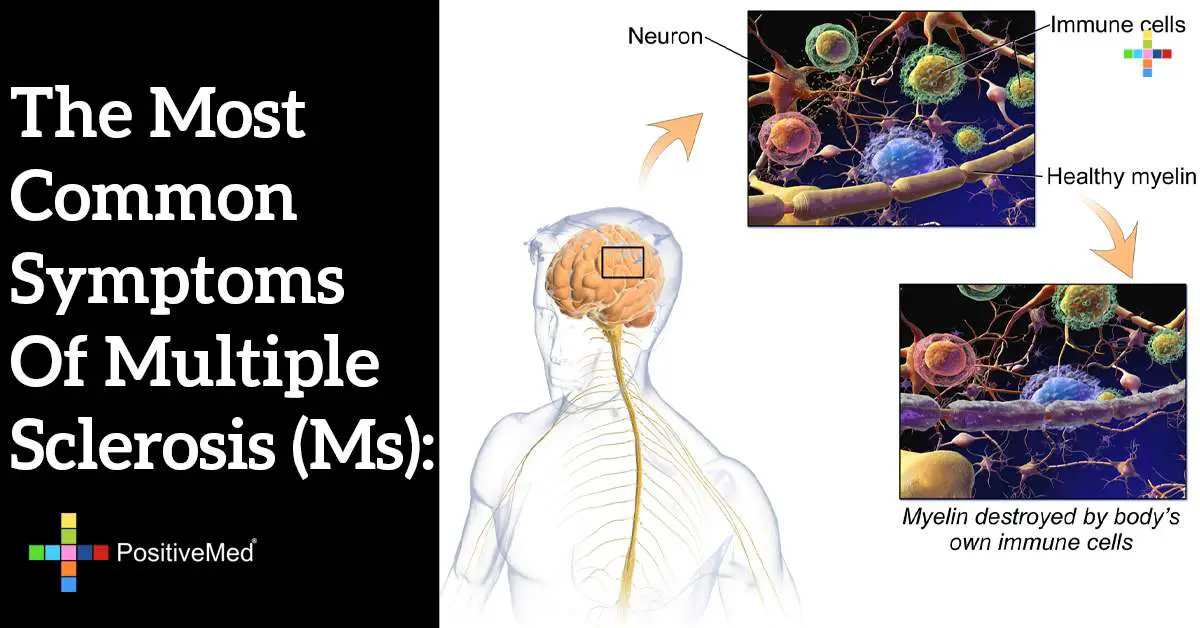
It is possible that ME/CFS is caused by a change in the persons immune system and the way it responds to infection or stress. ME/CFS shares some features of autoimmune illnesses . For example, both ME/CFS and most autoimmune diseases are more common in women and both are characterized by increased inflammation. However, other signs of autoimmune disease, like tissue damage, are not found in patients with ME/CFS.
Scientists think that the immune system might be contributing to ME/CFS in other ways, including:
Read Also: What Doctor Treats Chronic Fatigue Syndrome
Redox Imbalance In Me/cfs
In people with ME/CFS, there are multiple biomarkers of oxidative stress: reduced levels of antioxidants decreased levels of -tocopherol increased levels of peroxides and superoxide that correlate with severity of symptoms increased levels of isoprostanes, both at rest and after exercise and reduced levels of thiobarbituric acid reactive substances and malondialdehyde levels, as well as reduced ascorbic acid and glutathione levels . These markers of redox imbalance also correlate with severity of symptoms . Brain magnetic resonance spectroscopy reveals elevated levels of ventricular lactic acid consistent with oxidative stress .
When compared with healthy control subjects, people with ME/CFS also have multiple biomarkers of nitrosative stress: increased inducible nitric oxide synthase with consequent increased NO, peroxynitrite, and nitrate, particularly following exercise .
Immune responses to oxidized fatty acids and markers of lipid peroxidation also are significantly greater in ME/CFS patients as compared with controls .
Metabolomic studies in plasma from ME/CFS subjects are consistent with these findings, revealing altered plasma levels of choline, carnitine, and complex lipid metabolitesconsistent with oxidative stress and mitochondrial dysfunction .
Symptoms Of Chronic Fatigue Syndrome
The main feature of ME/CFS is a type of exhaustion known as post-exertional malaise, crash or payback. This means having flu-like symptoms after exercise and not having enough energy for daily activities.
Research shows that people with ME/CFS have a different physiological response to activity or exercise from other people. This includes abnormal exhaustion after any form of exertion, and a worsening of other symptoms. The response may be delayed, perhaps after 24 hours. Depending on the amount and type of exercise, it may result in post-exertional malaise for a few days, or serious relapses lasting weeks, months or even years.
- problems with thinking, concentrating, memory loss, vision, clumsiness, muscle twitching or tingling
- disrupted sleep
- sore throat, tender lymph nodes and a flu-like feeling
- inability to cope with temperature changes.
You May Like: Army Fatigue Jacket Forever 21
Molecular Mechanisms Behind Viral Pathogenesis In Me/cfs
Viral infection can initiate a multitude of physiological changes in host cells that can contribute to ME/CFS development . Viral pathogens frequently associated with ME/CFS are also known to alter various molecular processes in host cells that define clinical conditions of ME/CFS . Three of the most frequently discussed molecular processes, namely immune cell alterations, mitochondrial modulation and autoimmunity, are described in brief within this section.
Fig. 1
Schematic diagram showing various viral pathogens potentially associated with ME/CFS and possible molecular mechanisms altered by these pathogens that can contribute to ME/CFS development
The Overlap Between Long Covid And Chronic Fatigue Syndrome
Long COVID and ME/CFS , and this has inspired researchers to look into whether they could be linked. While its still early, researchers think that long COVID and ME/CFS share similar causes. More specifically, viral infection seems to cause both conditions , and may be the result of ongoing immune system dysfunction.
Similar to how COVID infection triggers long COVID, evidence suggests that ME/CFS may start with previous infection with a virus such as Epstein-Barr virus. But even after these infections are gone, researchers have found evidence that both ME/CFS and long COVID are associated with ongoing activation of the immune system. This may explain why people with these conditions experience symptoms that may resemble autoimmune disease.
So why does this ongoing immune dysfunction happen? Were not sure, but it may be related to the way both conditions have been linked to abnormally high immune system markers called cytokines. Studies suggest these cytokines play a role in the development of both ME/CFS and long COVID.
Its also unclear why this immune system response causes such profound fatigue, but one study of patients hospitalized for infection found that increased inflammation from the virus caused significant muscle weakness. This inflammation caused similar weakness experienced by those with ME/CFS.
But even though these conditions share certain similarities, it might be too soon to say for sure that they are the same.
Natural Supplements And Mitochondrial Dysfunction
A number of natural supplements have been used to treat nonpsychological fatigue and mitochondrial dysfunction.,, These supplements include those containing vitamins, minerals, antioxidants, metabolites, enzyme inhibitors and cofactors, mitochondrial transporters, herbs, and membrane phospholipids . Although several natural supplements have been used to reduce fatigue, few are considered truly effective. This article will discuss some of the most promising supplements and conclude with combinations of specific supplements that have been used to treat intractable chronic fatigue and improve mitochondrial function.
Where Can I Get Support
Even in its mildest form, chronic fatigue can have a significant emotional and financial impact on your life. A lack of understanding and awareness about CFS/ME means patients can experience disbelief, and even discrimination, from friends, family, health and social care professionals and employers.
People need wider support in order to continue to manage aspects of their life. Information on entitlements to welfare benefits, accessing health and social care and others sources of support for patients and carers are available from Action for M.E.
Action for M.E. has a number of booklets that may be useful for people living with CFS/ME, their families and their health professionals. They also offer resources and services for children and young people affected by chronic fatigue and their families.
Treating Chronic Fatigue Syndrome
Although there is no cure for chronic fatigue syndrome there are a number of ways to help manage your symptoms.
Because of the complexity of the illness, its changing nature and the number of possible symptoms, different things work for different people. Your GP may be able to support you through managing your individual symptoms. They may be able to refer you to a specialist service or to a service that will help you to manage individual symptoms but this depends on the services available in your area.
To decide what treatment is right for you, you should look at the evidence, including published research and patient surveys, and make sure you fully understand what the treatment involve, before you make a decision. You have the right to decline any treatment option you do not feel comfortable with.
Your GP may suggest some of the following treatment options.
What Is Chronic Fatigue Syndrome And What Are The Symptoms
Chronic fatigue syndrome , also known as myalgic encephalomyelitis , is a long-term condition that affects many systems in the body and results in debilitating fatigue that is often worse after activity. One report estimates that up to 2.5 million people in the U.S. suffer from ME/CFS, and that the condition is likely underdiagnosed.
While there are no tests to diagnose this condition, providers consider ME/CFS when someone experiences profound fatigue for more than 6 months with no other explanation. People with ME/CFS are unable to do their usual activities, and may even be bedbound. Their symptoms may get worse when they try to be active, a symptom called post-exertional malaise.
Other common symptoms of ME/CFS include:
-
Problems sleeping
-
Nausea, vomiting, or diarrhea
-
Recurring sore throat
If these symptoms sound familiar, its because many of them overlap with the symptoms of long COVID.
Dysregulated Heme And Iron Homeostasis
Increased levels of free iron in cells and increased ferritin levels both can cause oxidative damage . Iron stored in heme molecules is degraded via the bilirubin pathway, an important component of antioxidant defense . Evidence of dysregulated heme and iron homeostasis has been reported in acute COVID-19 and ME/CFS .
Future Strategies For Development Of Infection Biomarkers In Me/cfs
Use of quantitative assays rather than qualitative assays to assess the extent of the viral load instead of simple detection of presence or absence. This may facilitate monitoring of a response to treatment however, diurnal variations and individual response on treatment should be taken into account. Further comprehensive serological testing may help to identify a signature of active infection.
Use of additional biological samples together with blood and serum will be useful in determining the localization and distribution of biomarkers, as well as pathogenicity. Using hair follicles, virus integration can be detected. Similarly throat swab and stool samples can be used for detection of enteroviruses.
Functional studies to compliment clinical biomarker studies in order to clarify functions and interactions of genes, transcripts, proteins, and immune cells and molecules in cases of ME/CFS. This will facilitate understanding of the disease aetiology as well as development and maintenance pathways, and thereby, potential prevention and treatment strategies. However, this strategy requires definition of ME/CFS subgroups.
Use of high throughput methods to gain broader insight into potential biomarkers for infections by obtaining and analysing large-scale data, which will raise the quality and significance of the research.
Abnormal Metabolism Involving The Gaseous Signaling Molecules No And Hydrogen Sulfide
The major gaseous signaling molecules include NO, carbon monoxide, and hydrogen sulfide . They play key roles in the regulation of blood pressure, inflammation, and neurotransmission . Under physiological conditions, both NO and H2S have anti-inflammatory effects . However, both deficient and excess production of these gaseous signaling molecules can create brain pathology, immune dysfunction, and redox imbalance .
NO.
NOS2 is significantly up-regulated in patients with severe and critical COVID-19 . There is evidence of nitrosative stress and disordered NO metabolism in people with ME/CFS . Levels of NO are higher in ME/CFS patients, which can accelerate nitrosative stress . Citrulline, a product of arginine metabolism by NOS, also is increased in ME/CFS .
H2S.
Normal H2S metabolism protects against inflammation and redox imbalance . One of the modes by which H2S functions is by a posttranslational modification termed persulfidation or sulfhydration , which prevents irreversible oxidation of proteins . H2S metabolism is disrupted in Alzheimers disease, Parkinsons disease, and Huntingtons disease and also, during aging . H2S inhibits tau-phosphorylation, which may explain, in part, its role in protecting against Alzheimers disease .
