Autoimmune Disease Risk Factors
Researchers dont know what causes autoimmune disease, but several theories point to an overactive immune system attacking the body after an infection or injury. We do know that certain risk factors increase the chances of developing autoimmune disorders, including:
- Genetics: Certain disorders such as lupus and multiple sclerosis tend to run in families. Having a relative with autoimmune disease increases your risk, but it doesnt mean you will develop a disease for certain, says Orbai.
- Weight: Being overweight or obese raises your risk of developing rheumatoid arthritis or psoriatic arthritis. This could be because more weight puts greater stress on the joints or because fat tissue makes substances that encourage inflammation.
- Smoking: Research has linked smoking to a number of autoimmune diseases, including lupus, rheumatoid arthritis, hyperthyroidism and MS.
- Certain medications: Certain blood pressure medications or antibiotics can trigger drug-induced lupus, which is often a more benign form of lupus, Orbai says. Our myositis center also discovered that specific medications used to lower cholesterol, called statins, can trigger statin-induced myopathy. Myopathy is a rare autoimmune disease that causes muscle weakness. Before starting or stopping any medications, however, make sure to talk to your doctor.
Read Also: Is Fatigue A Symptom Of Prostate Cancer
What Symptoms Are Related To Joint Pain And Swelling
The symptoms of joint pain and swelling can vary from person to person, and depend on which joints are affected. The pain and swelling is often accompanied by stiffness, aches and a feeling of heat or warmth.
In some cases, it can lead to problems moving around, completing daily activities , and for some people, working.
Joint pain and swelling may be better or worse at different times of the day. For example, you may find that your joint pain and swelling is worst first thing in the morning. Pain and swelling in the joints can also lead to tiredness and fatigue.
The Flu Or Other Infections
When a flu virus hits, it brings on fever and congestion, and it can make your muscles ache, especially in your back, legs, and arms. It usually gets better on its own in a week or so, but call your doctor if it doesnât. You also should see them if you have other health problems and you get the flu or you have a cough that doesnât go away. Other infections can also give you muscle aches, including COVID-19 and HIV.
Read Also: Does Simponi Aria Cause Fatigue
Fatigue In Chronic Rheumatologic Diseases
Unusual and chronic fatigue with various etiologies was described for 27 % of patients in a primary care clinic . Fatigue is common in RA, SpA, Sjögren syndrome, systemic lupus erythematosus and vasculitis, although most publications concerned fatigue in RA or SpA . In RA and SpA, the frequency of fatigue ranged from 42 % to 80 % depending on the definition and methods of assessment . For 75 % of patients with ankylosing arthritis and 50 % of those with RA, fatigue was considered severe .
Several methods of evaluation have been used to investigate fatigue in rheumatologic diseases . The simplest and quickest scale is the visual analog scale , but this is a unidirectional scale. Multidirectional scales developed to include the different aspects of fatigue are the Medical Outcomes Study Short Form 36 vitality subscale , the Functional Assessment of Chronic Illness Therapy Fatigue Scale , the Profile of Mood States, the RA-specific Multidimensional Assessment of Fatigue scale, the Multidimensional Fatigue Inventory, the Brief Fatigue Inventory, and the Fatigue Severity Scale . With the VAS scale, the mean fatigue level in patients with RA was 42.1 .
What Can I Do
Therefore, ensuring that all your thyroid levels are optimal, supplementing magnesium, Vitamin D or using Epsom salts for baths/foot soaks and exploring whether you have adrenal issues and subsequently treating it, could help you resolve the symptoms. Low Free T3 levels in particular should be checked for and addressed.
Fluid retention, another somewhat common hypothyroid symptom, can cause pain, too. Its most often seen around the ankles and feet and worsens with physical activity. This is also often solved with optimal thyroid and vitamin levels.
Other short term treatments for hypothyroid myopathy can include massaging the affected area/s, which increases blood flow and eases aches and pains, or a warm bath/foot soak which helps to relax muscles, bonus points if you use Epsom salts, which is a popular trick for relaxing and relieving tired and achy muscles, among other things . You can get the ones I use by clicking here.
Magnesium spray or a Turmeric Supplement is also popular if you prefer to not add another supplement or tablet to your daily regimen and acupuncture has been helpful to some thyroid patients, too. A magnesium spray that is particularly popular with thyroid patients is this one.
Gluten-caused inflammation can cause joint and muscle pain in some people, too.
This site uses Akismet to reduce spam. .
You May Like: How To Stop Afternoon Fatigue
How Can I Best Learn To Cope With Musculoskeletal Pain
To help yourself cope with musculoskeletal pain:
- Avoid smoking, which increases inflammation.
- Eat a healthy, non-inflammatory diet.
- Rest the injured muscle, joint or bone.
- Stretch daily or as often as your healthcare provider advises.
- Take pain medications as prescribed.
- Use ice and heat to decrease swelling and inflammation.
A note from Cleveland Clinic
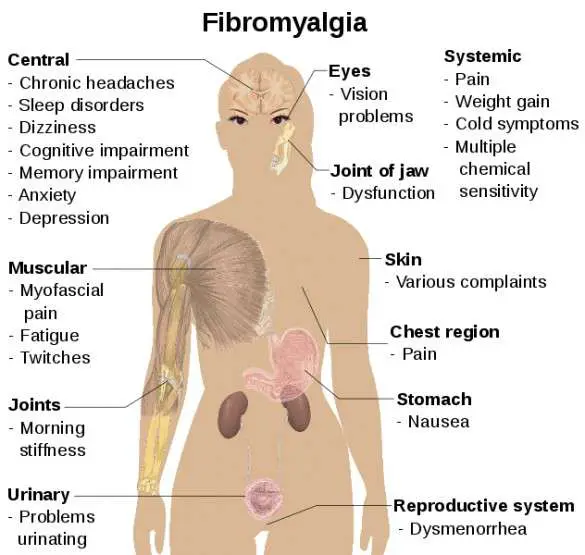
Musculoskeletal pain can cause discomfort and disrupt your daily activities. Sometimes, a sudden injury such as a broken bone causes severe pain. For some people, underlying conditions like arthritis or fibromyalgia lead to pain. Whether your musculoskeletal pain is acute or chronic, the right treatment can relieve your symptoms.
Last reviewed by a Cleveland Clinic medical professional on 03/10/2021.
References
Joint Pain And Swelling
Up to 90% of people with lupus will have arthritis, which is defined as inflammation or swelling of the joint lining. The most common symptoms of arthritis are stiffness and aching, most often in the hands and wrists. Symptoms of arthritis can come and go and move from one joint to another. Pain and stiffness tend to be worse in the morning and improve as the day goes on. People with lupus can also experience pain in the joints without swelling or tenderness, which is referred to as arthralgia.
Recommended Reading: Chronic Fatigue And Immune Dysfunction Syndrome
Sjogrens Syndrome As A Cause Of Joint Pain And Fatigue
Those diagnosed with Sjogrens Syndrome result in the immune cells attacking the glands that help in producing saliva and tears.
The disorder has an adverse effect on the kidneys, liver, lungs, pancreas and brain. It also results in arthritis and fatigue. Lymph nodes could swell and one may be at a higher risk of lymphoma. Sometimes, the disorder accompanies autoimmune diseases like lupus and rheumatoid arthritis.
What Causes Autoimmune Diseases
The precise cause of autoimmune diseases is unknown. However, there are risk factors that may increase your chances of getting an autoimmune disease. Risk factors include:
- Some medications. Talk to your healthcare provider about the side effects of medications for blood pressure, statins and antibiotics.
- Having relatives with autoimmune diseases. Some diseases are genetic they run in families.
Read Also: Consumer Reports Anti Fatigue Mats
Can Anyone Experience Lingering Covid
When it comes to the life-threatening cases of COVID-19, doctors expect people who were hospitalized for severe pneumonia or stroke to need specialized care and frequent follow-up after being discharged.
But, although not completely defined just yet, post-COVID syndrome isnt exclusive to people who experienced organ damage during their illness. Its also not exclusive to people whose symptoms warranted a trip to the emergency room.
Post-COVID syndrome can be seen in people who went to the ER with concerning symptoms or who had advanced symptoms that required a brief hospital stay, but it can also occur in people who had mild symptoms and self-treated at home, warns Dr. Lahoti. The important thing to note is that these are people who might not have required care from a specialist during their actual illness, but may now benefit from specialized care as these lingering symptoms continue to affect their daily lives.
The actual frequency of post-COVID syndrome is still largely up for debate, and different studies find this condition to be more or less common in various groups of people.
Some studies show that only 10% of people with COVID will go on to develop post-COVID syndrome, while other studies are showing much higher percentages some even suggest that up to 70% of people experience persistent symptoms, says Dr. Lahoti.
According to Dr. Lahoti, there are hints and suggestions as to whos most likely to develop lingering symptoms, though.
Did You Start To Experience Any Additional Arthritis Symptoms
I went to my GP a handful of times as I had been having a few difficult months and every time my bloods were okay. I was then referred to rheumatology, offered counselling and anti-depressants. Also, I was advised to go back on amitriptyline due to my pain and fatigue levels.
The next time I called my surgery, I spoke to a female GP and she said, Has anyone spoken to you about menopause? and I said, No, I havent thought about it.
We had a fantastic conversation and she suggested that I start on the HRT pill first, this did nothing and so I went onto the HRT patch. I didnt know what to expect as I didnt know if the pain and fatigue were due to my arthritis or something else.
Gradually, I noticed my mood lift, and this helped me to manage my pain better. I decided to come off the contraceptive pill after I had advice from a homeopath who I met at a networking event. I didnt have a period, only some initial spotting on and off and period pain.
I had lost my sex drive and that has come back since being on the HRT patch!
You May Like: What Can You Do To Combat Fatigue
Don’t Miss: Best Adaptogenic Herbs For Adrenal Fatigue
Disease Activity And Fatigue
Fatigue and arthritis go hand in hand for many people with arthritis. The main culprits are the inflammatory disease process and the accompanying chronic pain.
- Inflammation. If you have an autoimmune disease, your immune system attacks your body and inflammation is the result. The body undergoes stress as it tries to cope with the release of inflammatory cytokines in the blood. That can cause fatigue, especially when disease activity is high or low-grade inflammation remains for a long time.
- Chronic Pain. The pain-fatigue connection can be a vicious circle. Dealing with arthritis pain for months at a time over many years can wear you down. It can affect your sleep habits, which adds to your exhaustion. Being fatigued, in turn, can worsen pain and make it more difficult to manage.
Learn How To Control Stress
When a person is under excessive stress, breathing becomes more shallow, limiting oxygen that’s available to the body. Start breathing deeply to consciously ward off the effects of stress. Take 5 or 10 deep breaths when you feel stressed and fatigued. Breathing exercises and meditation are techniques you can practice any time practicing them will arm you with the tools you need to react to stress and fatigue.
Also Check: What Causes Fatigue And Weakness
Develop Good Sleep Habits
There are well-known sleep tips, and you should follow themgo to bed at the same time each night, get up at the same time each day, establish a ritual so that your body will recognize its time to sleep . If you still have trouble falling or staying asleep, you may wish to discuss sleep medications with your healthcare provider.
Recommended Reading: Can Fatty Liver Cause Extreme Fatigue
Polymyalgia Rheumatica And Giant Cell Arteritis
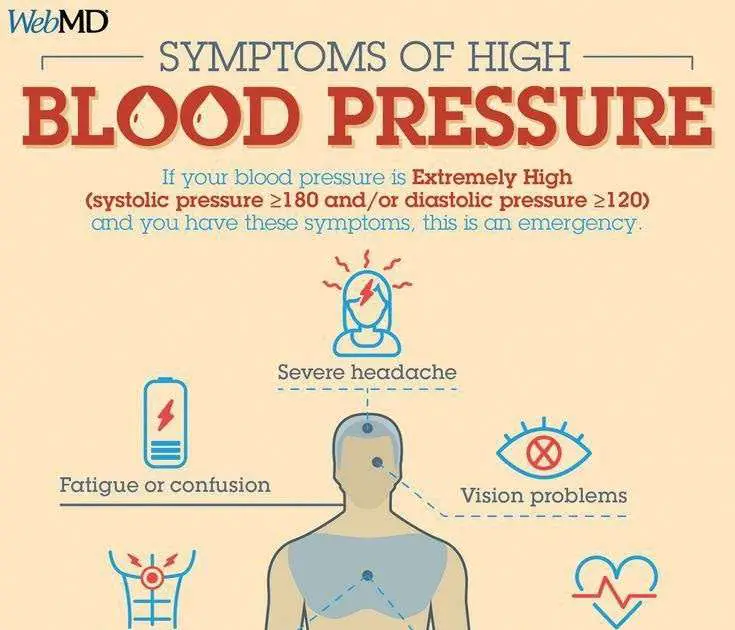
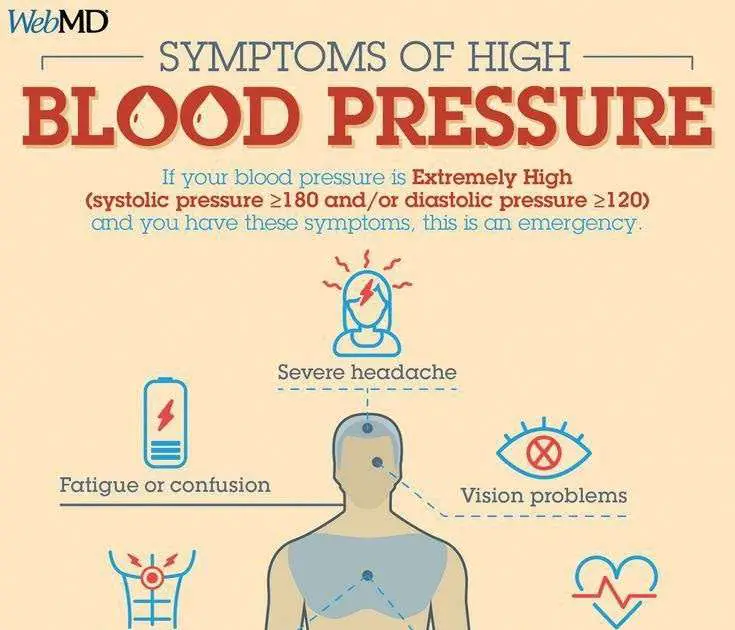
Some people with polymyalgia rheumatica experience giant cell arteritis . Giant cell arteritis involves painful inflammation of the blood vessels of the skull. Symptoms include:
- severe headache
- pain in the side of your jaw or face when chewing
- temples are tender to touch
- scalp tenderness.
Seek urgent medical attention if you experience any of these symptoms. If not treated promptly, giant cell arteritis can cause damage to the arteries of the eye, which can lead to blindness.
You May Like: Chronic Fatigue Syndrome In Men
Disease Activity And Sleep
Fatigue and sleep problems go hand-in-hand for many people with arthritis. The main culprits are the inflammatory disease process and the accompanying chronic pain.
- Inflammation. If you have an autoimmune disease, your immune system attacks your body and inflammation is the result. The body undergoes stress as it tries to cope with the release of inflammatory cytokines in the blood. That can cause fatigue, especially when disease activity is high or low-grade inflammation remains for a long time.
- Chronic Pain. The pain-fatigue connection can be a vicious circle. Dealing with arthritis pain for months at a time over many years can wear you down. It can affect your sleep habits, which adds to your exhaustion. Being fatigued, in turn, can worsen pain and make it more difficult to manage.
Symptoms By Autoimmune Condition
There are more than 80 autoimmune conditions. There is an overlap in symptoms among many of these conditions, and distinctive symptoms can help differentiate between them.
If you have one autoimmune disease, you have a 25% chance of developing other autoimmune conditions. This can make sorting out diagnoses more difficult. It can also cause some symptoms to be compounded.
Recommended Reading: Joint Pain Muscle Pain Fatigue
What Is The Prognosis For These Diseases
In most cases, the symptoms of dermatomyositis resolve with therapy. The disease is usually more severe and resistant to therapy in individuals with heart problems. Approximately one-third of individuals with juvenile-onset dermatomyositis recover from their illness, one-third have a relapsing-remitting course of disease, and the other third have a more chronic course of illness.
The prognosis for polymyositis varies. Most individuals respond fairly well to therapy, but some people have a more severe disease that does not. These individuals may have significant disability. Since polymyositis can cause difficulty swallowing, people can become malnourished. They are also at increased risk for falling, which can lead to hip and other bone fractures, disability, or death. In rare cases people with severe and progressive muscle weakness can develop respiratory failure or pneumonia.
Although necrotizing autoimmune myopathy is more difficult to treat than polymyositis and dermatomyositis, it generally responds well to long-term combination immunosuppressive therapies.
IBM is generally resistant to all therapies and currently available treatments do little to slow its progression.
Symptoms Of Autoimmune Myositis
) and may include vomiting of blood, black and tarry stools, and severe abdominal pain, sometimes with a hole , which causes a release of gastrointestinal contents and can lead to sepsis ⦠read more ) in the lining of the bowel.
Skin changes occur in people who have dermatomyositis. Rashes tend to appear at the same time as muscle weakness and other symptoms. A dusky or purplish rash can appear on the face with reddish purple swelling around the eyes. The rash may also be raised and scaly and may appear almost anywhere on the body but is especially common on the knuckles, elbows, knees, outer part of upper thighs, and parts of the hands and feet. The area around the nails may redden or thicken. When the rash fades, brownish pigmentation, scarring, shriveling, or pale depigmented patches may develop on the skin. The rash on the scalp may look like psoriasis and be intensely itchy. Sun sensitivity and sores on the skin occur as well. Bumps composed of calcium may develop under the skin or in muscle, particularly in children. Raised, reddish bumps may appear on the large knuckles and sometimes on the small knuckles.
Sometimes these characteristic skin changes occur in people who do not have muscle weakness and inflammation. In this case, the disorder is called amyopathic dermatomyositis.
You May Like: Can Doctors Test For Adrenal Fatigue
How Are Autoimmune Diseases Treated
There are no cures for autoimmune diseases, but symptoms can be managed. Everyones immune system, genetics and environment are different. That means that your treatment must be unique.
Some examples of medications used to treat autoimmune diseases include:
Dont Miss: How Long Does Gluten Fatigue Last
What Can Be Done
- Persistent joint and muscle pain should never be ignored
- If even after 4-6 months post Covid, you are having persistent pain it needs to be investigated
- If the patient suffered from autoimmune arthritis then a rheumatologist must be involved
- While the degeneration cannot be reverse, treatment should be initiated to halt or slow down the process.
- While some of the post-Covid symptoms will heal on their own in time, there are others that must not be ignored. One must take care of physical fitness and nutrition intake during the recovery process for long-term good health.
Read Also: Chronic Fatigue Syndrome Home Remedies
Recommended Reading: Lower Back Pain And Fatigue
Nerve Conditions Which Damage Muscles
Conditions affecting nerves tend to lead to true muscle weakness. This is because if the nerve to a muscle fibre stops working, the muscle fibre cant work either and it will become floppy and eventually shrivel.
Neurological conditions: muscle weakness can be caused by cerebrovascular disease such as stroke and brain haemorrhage and spinal injury. Tumours in the brain can also lead to muscle weakness. Muscles which become partially or completely paralysed lose their normal strength and will eventually waste. Some recovery is possible but it will be slow and may not be complete.
Spine-related conditions: when nerves are damaged as they emerge from the spine , weakness can result. When the discs slip out, they press on nerves headed lower down in the body. The weakness affects only the muscles served by the irritated or compressed nerve.
Other uncommon nerve conditions:Multiple sclerosis : this is caused by damage to nerves in the brain and spinal cord and can cause sudden paralysis. This can recover partially but does not always do so.
: this is a post-viral paralysing disease which causes weakness and loss of muscle function from the fingers and toes upwards. It may last many months, although complete recovery is usual.
