Ways To Reduce Alarm Fatigue In Hospitals
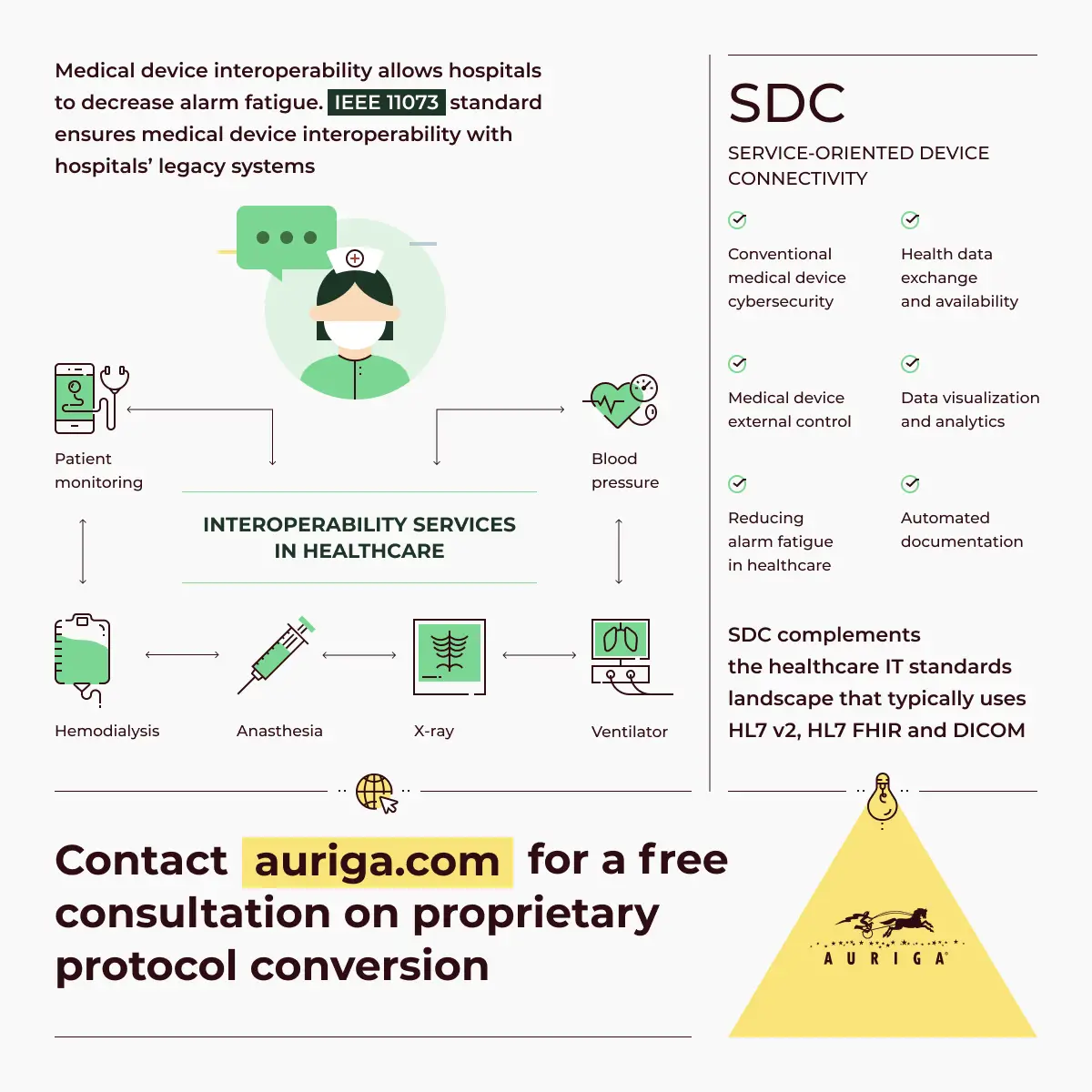
The sheer volume of alarms in the typical hospital room causes alarm fatigue: Clinicians experience sensory overload from the excessive number of alarms and become desensitized, which can lead to longer response times or critical alarms being missed altogether.
According to The Joint Commission, alarm alert and notification overload is one of the top ten health technology hazards in healthcare. No matter the size of the hospital, chances are high that you are exposed to the sounds of alarms beeping and buzzing all day long. Modern hospitals foster a highly computerized clinical environment, resulting in nearly everything being hooked to a monitor that can make audible noisesreal or false.More than 19 in 20 hospitals are concerned with alarm fatigueand the potentially detrimental effect it can have on patient safety.
A study at Johns Hopkins Hospital found that 350 alarms were produced per bed during a single day in an intensive care unit. When alarms function as intendedsounding when medical action should be takenpatient safety is enhanced. However, alarms sounding all day, every day, lead to such extreme desensitization that many alarms simply arent heard, they are disabled, or they arent triaged appropriately.
1. Clean and monitor the equipment
2. Decrease clinically inconsequential alerts
3. Funnel alerts to the right people
4. Triage alerts with software
5. Get rid of the noise
6. Tailor alerts to patient characteristics
7. Invest in advanced clinical alerting
Route Calls Or Alerts To The Right Person/role
Routing calls or alerts to the right people or roles can reduce the number of alerts that interrupt the nurses and the staffand the nurse call system is where your organization can be savvy aboutpreserving nurses’ focused time. Alternatives include routing calls to a unit clerk, care assistant, or the whole unit.
Gaps And Future Directions
The current literature on this PSP primarily concerns QI initiatives and case studies higher quality studies could help to better understand the impact of implementing elements of safety culture to address alarm fatigue. In addition, because efforts to improve safety culture typically involve multiple elements and are often part of a larger hospital-wide initiative, it is difficult to know which intervention are most responsible for reducing alarm fatigue. The studies we reviewed had small sample sizes and focused on one hospital or specific unit, and often one type of monitor/alarm, and may have limited generalizability.
Read Also: Latest News On Chronic Fatigue Syndrome
Agency For Healthcare Research And Quality
5600 Fishers Lane
- Don’t have account?Create new account
Submit Your Case
Please select your preferred way to submit a case.
Continue as a Guest
Track and save your case in My
Cases
Edit your case as a draft
Your name will not be publicly
associated with the case
Track and save your case in My
Cases
Edit your case as a draft
Your name will not be publicly
associated with the case
Submit Your Case
Please select your preferred way to submit a case. Note that even if you have an account, you can still choose to submit a case as a guest. And if you do choose to submit as a logged-in user, your name will not be publicly associated with the case. Learn more information here.
Continue as a Guest
Impact Of Alarm Fatigue On The Work Of Nurses In An Intensive Care Environment
Lewandowska K, Weisbrot M, Cieloszyk A, et al. Impact of alarm fatigue on the work of nurses in an intensive care environment–a systematic review. Int J Environ Res Public Health. 2020 17:8409. doi:10.3390/ijerph17228409.
Alarm fatigue, which can lead to desensitization and threaten patient safety, is particularly concerning in intensive care settings. This systematic review concluded that alarm fatigue may have serious consequences for both patients and nursing staff. Included studies reported that nurses considered alarms to be burdensome, too frequent, interfering with patient care, and resulted in distrust in the alarm system. These findings point to the need for a strategy for alarm management and measuring alarm fatigue.
Read Also: Supplements For Hashimoto’s Fatigue
Which Providers Or Roles Receive Alerts
Alerts are typically directed at roles in the nursing unit and can include nurses, unit clerks, and patient care techs Respiratory therapists and other ancillary team members also receive various types of alerts, but alarms that become alerts will always go to a nurse. If the nurse doesnt respond, the alert should escalate to another nurse or a charge nurse. In addition, all physiologic monitor alerts go to nurses. Therefore, nurses should receive only the most important interruptions from devices.
A Nursing Program Designed For You
Ohio Universitys online MSN program prepares registered nurses and other Bachelor of Science in Nursing graduates for a variety of advanced nursing careers, including to assume the role of an APRN.
The program concentrations enable nurses to specialize their education in their areas of interest. Concentrations include: Family Nurse Practitioner, Nurse Educator, Adult-Gerontologic Acute Care Nurse Practitioner, and Psychiatric Mental Health Nurse Practitioner.
For more information about the Ohio University online MSN program, visit the program webpage today for the full curriculum and other details.
Don’t Miss: What Deficiency Causes Tiredness And Fatigue
What Is Alarm Fatigue For Nurses
In healthcare, we talk about the dangers of alarm fatigue and its consequences: It presents a threat to patients when an alarm is overlooked, and unrelenting alarms and alerts exact a toll on clinicians.
Not unlike the boy who cried wolf, as Nadine Salmon wrote on rn.com, the constant drone of beeps and buzzes, not to mention false alarms in between, can leave todays healthcare provider desensitized and in danger of missing the next alarm.
Shes right. Ive been there.
All clinicians struggle with alarm fatigue, but in this article, I address it from a nurses perspective. I’ve worked with alarms and alerts within acute settings as a caregiverand as part of a team that comes in to provide solutions to reduce the number of alarms and alerts directed at clinicians.
Education Can Help Nursing Staff Gain Control And Improve Patient Safety
Takeaways:
- A standardized unit-based education program increases nurse awareness of clinical alarm fatigue.
- Nurses become desensitized to noise created by audible nonactionable alarms.
Someone with an outside perspective may be surprised by the noise and chaos of an intensive care unit , where alarms go off repeatedly. But nurses and others who work in that environment every day too often think the chaos is normal, when in fact its creating distraction and jeopardizing patients.
Alarms have a long history of compromising patient safety, and recent studies demonstrate the negative consequences alarms have on families and nurses as well. To highlight the importance of this issue, for the fifth year in a row, reduction of clinical alarm harm is a Joint Commission National Patient Safety Goal.
To address this problem, a team of interdisciplinary professionalsincluding human factors engineers, clinical engineers, a unit-based nurse manager, a unit medical director, a unit-based clinical nurse specialist, a central nursing clinical nurse specialist, and expert bedside nursesat a large academic medical institution launched a quality improvement project to look into the effects of alarm fatigue and strategies to reduce the number of nonactionable alarms.
Recommended Reading: Can Fatigue Cause Rapid Heart Rate
A Few Scary Facts About Hospital Alarms
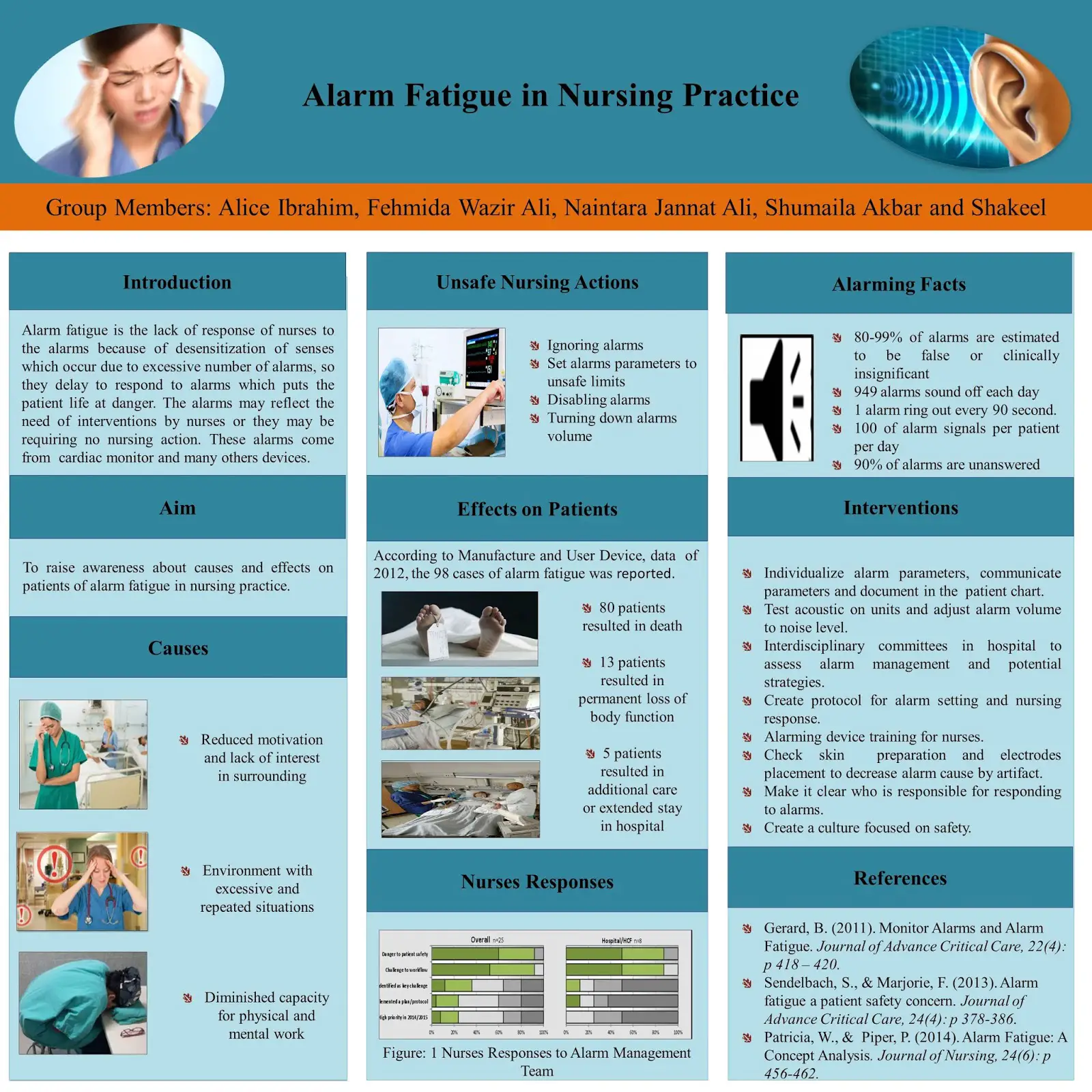
Alarm fatigue is one of the most troubling and highly researched issues in nursing. Over the last decade, research has found the following staggering statistics related to alarm fatigue and false alarms:
- The Food and Drug Administration reported more than 560 alarm-related deaths in the United States between 2005 and 2008.
- Between January 2009 and June 2012, hospitals in the United States reported 80 deaths and 13 severe injuries.
- One study showed that more than 85 percent of all alarms in a particular unit were false.
- A hospital reported an average of one million alarms going off in a single week.
- A childrens hospital reported 5,300 alarms in a day 95% of them false.
- A hospital reported at least 350 alarms per patient per day in the intensive care unit.
Establish Policies And Procedures For Managing Important Alarms
When alarms go off, its important to know exactly how they should be managed or addressed. There are several aspects that must be questioned regarding alarm procedures to prevent alarm fatigue and patient safety.
- What are the clinically appropriate settings for alarm signals
- When alarm signals can be disabled
- When alarm parameters can be changed
- Who in the organization has the authority to set alarm parameters
- Who in the organization has the authority to change alarm parameters
- Who in the organization has the authority to set alarm parameters to off
- How to monitor and respond to alarm signals
- How to inspect individual alarm signals for accurate settings, proper operation, and detectability
Its also important to educate staff and licensed independent practitioners about what alarm fatigue is, and the purpose and proper operation of alarm systems for which they are responsible.
Hospitals themselves may be able to diagnose the cause of nuisance alarms that do more harm than good. In 2019, Seattle Childrens Hospital established a protocol for their team of respiratory therapists. It developed high and low limits for device alarm settings, as well as allowed professionals to make adjustments to the devices if necessary to reduce ongoing errant alarms.
Don’t Miss: Causes Of Chronic Fatigue And Sleepiness
Improve The Nursing Environment And Ensure Patient Safety As A Nurse Leader
Nurse leaders play an important role in shaping the future of healthcare. With the right education and preparation, they have an opportunity to create safer, more productive working environments for professionals across the industry.
program is designed to help nurses advance their careers by practicing evidence-based decision-making, focusing on the tenets of preventive and compassionate care, and gaining clinical experience in their preferred settings. Students can also choose from five nurse practitioner concentrations, allowing them to pursue the track that best meets their passions and career goals.
Act today to learn how Maryville can help you become a nurse leader and innovator.
Recommended Reading
What Can Be Done To Combat Alarm Fatigue
While it may be easy to blame the bedside caregivers for not responding to alarms, its important to understand that alarm fatigue needs to be addressed at the administrative level. Implementing an enterprise-wide patient safety solution, these healthcare facilities can decrease the frequency of false alarms.
The smartest patient safety investment would combine real-time location system technology with a proven security system. These solutions can provide location information wherever 100% accuracy is needed including rooms, hallways, beds, chairs, bassinets and even bays. So how does this fight against alarm fatigue? Lets say a patient is standing by the door inside of their room. A clinical-grade patient safety system would show with certainty that the patient is still safely inside their room while an estimated-locating solution may mistakenly set off an alarm thinking that he or she was in the hallway. This avoids another unnecessary alarm and helps prevent further alarm fatigue.
Don’t Miss: How To Combat Fatigue From Kidney Disease
Technological Advances In Patient Monitors
In general, clinical monitoring is based on a careful balance between sensitivity and specificity of alarm signal recognition, as well as the associated threshold setting required to trigger alert condition . Increasing monitor sensitivity helps ensure that truly significant events are not missed, primarily using single-parameter alarms and default thresholds . However, as a trade-off this increases the incidence of nuisance alarms that are nonactionable. This issue may be remedied by the development of smart alarm systems that use algorithmic approaches to evaluate multiple parameters prior to determining whether the detected change is truly critical, and only then sending an alert to the operator . This improvement in device specificity would result in significantly fewer false alarms and therefore reduce AF. At the same time, the challenges of unpredictable code and interrupted or corrupt data have been noted and may represent an important safety issue due to the potential for missing data or data misinterpretation, especially when using memory-intensive applications on devices that are continually operating for prolonged periods of time .
| System |
|---|
Burdensome And False Alarms
In studies carried out by Christensen et al., 59% of questioned nurses reported that the inconvenience of alarms results from incorrectly set alarm thresholds . In addition, 95% of nurses declared that they often felt the burden of alarms . The inconvenience of alarms causes disturbances in the care of patients . Importantly, the nuisance and falsity of alarms result in a reduction of trust in monitoring systems . As a consequence of the large number of false alarms, nursing personnel are not capable of reacting to them in the proper manner . According to the studied nurses, modern technologies are too complicated, while false alarms are too frequent and distract their attention .
Don’t Miss: Does Skin Cancer Cause Fatigue
More Than Just A Nuisance
The proliferation of alarms generated by monitoring systems is a growing concern for anyone committed to patient safety. Exposure to excess alarms in care settings, especially non-actionable alarms, can result in desensitisation among the clinicians that they are intended to alert, a syndrome called alarm fatigue. Alarm fatigue can lead to reflexive silencing of alarms, breaking monitoring protocols and missing true positive alarmsplacing a burden on caregivers and jeopardising their ability to care for patients.
When an alarm goes off you want to make sure it is clinically relevant.
Ineke van de Pol
ICU nurse practitioner, St. Antonius Hospital, The Netherlands
Alarm Fatigue A Top Patient Safety Hazard
CMAJCopyright
Medical device alarms are designed to save lives, but excessive and misleading alerts remain a leading technological hazard in hospitals.
Clinical devices sound hundreds of alarms per patient per day, creating a cacophony that can overwhelm, distract and desensitize health workers, the US Emergency Care Research Institute reveals in its report, 2014 Top 10 Health Technology Hazards.
Caregivers with alarm fatigue are more likely to ignore or have trouble distinguishing between alarms, which can lead to delayed treatment and patient harm, the US Food and Drug Administration cites a report indicating there were 566 alarm-related deaths between 2005 and 2008. In the same period, Health Canada received 16 voluntary reports from hospitals of incidents tied to cardiac monitor alarms.
Addressing alarm fatigue is like opening Pandoras box, says Maria Cvach, the nurse lead of the alarm committee at Johns Hopkins Hospital in Baltimore, Maryland. There are so many different arms to the problem.
One is the sheer number of bells, beeps and chimes that echo through the modern hospital. A 12-day alarm system analysis at Johns Hopkins indicated there were an average 350 alerts per bed per day. In one intensive care unit, the average was 771 alerts per bed per day.
Adding to the confusion, theres no standardization of alarm sounds between device manufacturers, making it difficult for health workers to triage their response to alerts.
You May Like: Best Vitamins To Take For Fatigue
Alarm Fatigue And Patient Safety
View all blog posts under Articles | View all blog posts under Online Master of Science In Nursing
More technology is used in health care today than at any other time in history. It has made nurses jobs easier and helps keep patients alive longer. But it has also led to some unintended consequences.
Nurses who are caring for patients can become desensitized to the beeps and buzzes of medical devices often made in error. This, in turn, has caused health care organizations to be concerned over the link between alarm fatigue and patient safety. And with good reason.
Not responding to alarms can lead to critical patient safety issues, including medical mistakes and even death. The Joint Commission, a major health care accreditation body, indicates that between January 2009 and June 2012, there were 80 recorded deaths related to alarm fatigue
Earning an advanced degree, such as a Master of Science in Nursing , and becoming familiar with the dynamics of alarm fatigue, is essential for nurse leaders who want to be part of developing solutions to the issue.
Patient Monitoring: Different Types And Modalities
A diverse number of patient monitors are widely used across various health-care settings . When employed correctly, they provide potentially valuable, actionable, and real-time information about a patients clinical status. Different monitoring devices are intended to measure different parameters, potentially allowing for rapid assessment of a patient. This is especially relevant in the context of the current discussion of AF and more specifically the domain of alarm trigger accuracy . As clinical monitoring becomes more sophisticated and better integrated, remote implementations also become possible . The subsequent discussion will outline major types of monitoring equipment and alarms, including ventilation/oxygenation, hemodynamic, and pressure point alert systems.
Also Check: Anti Fatigue Blue Light Glasses
The Challenge Of Technology
The first barrier to implementation is the technology itself. Hospitals must recognize that monitoring devices often come with all alarms turned on and therefore invest the time to determine what actually must be alarmed on a particular unit. Fortunately as manufacturers have gotten more attuned with alarm fatigue, they have developed a better understanding of what typical alarms would be seen in particular hospital areas such as an intensive care unit versus an emergency department. Because of this, while all features are still included in the monitors, they are not necessarily activated unless you choose to.
Ways To Reduce Alarm Fatigue

It is important to acknowledge that while there is no universal solution to alarm fatigue, approaches must be made to combat it. Standardization can be customized for specific units and certain groups of patients.
The Association for the Advancement of Medical Instrumentation formulated the following recommendations to overcome alarm fatigue:
- Review and adjust default parameter settings and ensure appropriate settings for varying clinical areas
- Determine if certain alarms are not clinically significant and needed
- Implement procedures that allow staff to customize alarms based on each patients condition
- Ensure that all equipment is managed and maintained properly in order to work effectively
While nurses and healthcare employees are fully aware that alarms are unavoidable in hospital settings, it is of equal importance to understand the necessity of developing effective strategies to manage alarms. Nursing personnel can easily feel overburdened and overstimulated with an excessive number of medical duties along with a continuous wave of alarms.
Many nurses also do not realize the importance or the need for education regarding alarms which is a necessary element of any alarm management strategy system. Many hospitals and facilities do not assess the level of alarm fatigue and this is an area that needs to be focused on more intently.
You May Like: Best Anti Fatigue Mat For Standing