What Is Myalgic Encephalomyelitis/chronic Fatigue Syndrome
Myalgic encephalomyelitis/chronic fatigue syndrome is a complex and disabling disease. It has been classified as a neurological disorder by the World Health Organization, though it affects many parts of the body, including the brain and muscles, digestive, immune and cardiac systems.
The term myalgic encephalomyelitis means pain in the muscles, and inflammation in the brain and spinal cord. Scientists are starting to understand some of the biological changes in the bodies of people with ME/CFS, although they have not yet found how to prevent, or cure it.
Research has found that ME/CFS is associated with problems involving:
- The bodys ability to produce energy at a cellular level
- Immune, neurological and hormonal systems
- Blood pressure and heart rate regulation
- Cognition how quickly information is processed
ME/CFS affects men, women and children of all ages, ethnicities, and socioeconomic backgrounds. 75-80% of people with the disease are female. It is estimated that up to 600,000 Victorians may be living with ME/CFS, and as many as 90% are undiagnosed.
The Role Of The Microbiome In Cfs
The most current research assessing gut dysbiosis in CFS is coming out of Columbia University, New York. Findings have been considered a significant breakthrough in establishing biomarkers of disease. The study examined 100 people and showed those with CFS had a decreased microbial diversity and altered metabolic pathways, even in patients who did not display symptoms of IBS.
While this is most definitely not the first time the association has been investigated, it does appear to support and build upon previous research, which is a cause for some form of celebration, considering the heterogeneity of the disease.
IBS as a comorbidity is extremely common, with up to 90% of all patients also being diagnosed with IBS either before or after onset of symptoms of CFS. The research from Columbia University set out to delve further into the already emerging role gut bacteria and their metabolites play in disease progression outside of localised pathology, such as in central nervous system, immune and cognitive dysfunction.
Stool analysis showed the number and diversity of bacterial families Lachnospiracea and Porphyromonadaceae in CFS patients to be decreased, with abundant Clostridiaceae compared with controls. A decreased number of the genera Faecalibacterium and the increased colonisation of Alistipes were found to be predictive of CFS development and increased severity of symptoms.
What Are The Symptoms Of Chronic Fatigue Syndrome
Symptoms of CFS often mimic the flu. The following are the most common symptoms of CFS. However, each person may experience symptoms differently. Symptoms may include:
- Sensitivity to light
- Low-grade fever
The symptoms of CFS may look like other medical conditions. Always talk with your healthcare provider for a diagnosis.
Also Check: How To Combat Ms Fatigue
Which Facts Do Not Fit Into The Explanatory Model
Even if ME/CFS is of autoimmune origin, is it the metabolic block or the autoantibodies to hormone receptors which are most important for pathogenesis?
The mechanism behind the flare after exercise is obscure. Maybe a mitochondrial defect can lead to an increased activity in the innate immune network.
The disturbance in one-carbon metabolism may or may not be related to the disturbed transition between glycolysis and TCA cycle. It is indicative of a wider metabolic derangement than a block of PDH would be expected to lead to. There are several papers on hormones , including glucocorticoids and transient receptor potential channel hormones , and their receptors , in ME/CFS. It is conceivable that parts of the autonomic dysfunction can be explained in this way.
Is Analysis By Disease Severity Promising
At the Human Immune Monitoring Center at Stanfords Institute for Immunity, Transplantation and Infection, Dr. Montoya and his colleagues examined blood samples collected from 192 CFS/ME patients and 392 participants who had no CFS/ME diagnosis, or the control group.
All of the participants were aged 50 on average, and the diagnosed patients had lived with their symptoms for more than 10 years on average. The study took into account the severity of the patients condition, as well as how long they had been living with it.
The researchers found that participants with mild CFS/ME exhibited lower cytokine levels than the participants in the control group, whereas patients with more severe forms of the condition had elevated cytokine levels.
Dr. Montoya explains that these results may indicate different levels of genetic predisposition to the disease in its milder versus acute forms in the participants.
ts possible that for certain pathologies in humans, analysis by disease severity or duration would be likely to provide further insights, he suggests.
Those with a CFS/ME diagnosis, when compared with control group participants, also exhibited another important characteristic: a protein involved in cell differentiation and proliferation called
contexts , as in the case of some cancers.
Another pro-inflammatory cytokine correlated with severe CFS/ME was leptin , which also plays an important role in creating a feeling of satiety, telling us when we should stop eating.
Also Check: Does Chronic Fatigue Syndrome Qualify For Disability
Children Young People And Me/cfs
ME/CFS can affect people of all ages, including the very young. Young people with ME/CFS, especially children under the age of ten, might have trouble knowing or articulating that something is wrong. They may not realise that their loss of stamina, or other symptoms they are experiencing, are not normal. Alternatively, they may not have the words to describe what they are feeling.
For both younger children and teenagers, schooling can be affected but ME/CFS is not school refusal. While school refusal can often be accompanied by physical complaints , and these complaints may tend to disappear when the young person stays home, the pattern is different with ME/CFS. In a young person with ME/CFS, some symptoms never ease and symptom exacerbation is triggered by activity. In ME/CFS, symptoms are likely to be worse after school attendance, and can reduce with pacing and rest, which includes time away from school or during holidays.
Some young people with ME/CFS can continue to attend school, and others may be too unwell for regular classroom attendance. Parents, healthcare providers, schools and the child or teenager need to work together to come up with a plan for the young persons continued education. This plan needs to take into account the energy limits of ME/CFS. Being creative and flexible is key and might include things like fewer subjects or school from home.
Neutrophils In Autoimmune Diseases
Neutrophils are innate immune cells derived from common myeloid progenitor cells in the bone marrow . Neutrophils are important in defending the body against antimicrobial pathogens in the presence of various receptor recognition pathways. Activated neutrophils contain factors that are released into the phagosome during pathogen infiltration these include azurophilic, explicit or secondary, gelatinase granules and secretory vesicles . Derivatives of these neutrophil compartments are discharged via degranulatioin causing destruction of microbes, modifications in cytokines, chelation of microbial nutrients and heightened sensitivity to inflammatory response . Reactive oxygen species are also generated via oxidative phosphorylation in the neutrophil phagolysosome to ensure effective clearance of pathogens.
In CFS/ME, neutrophils have been reported to be highly susceptible to apoptosis in the presence of increased incidence of TNFR1 and TGFβ1 . Deregulation in neutrophil function may however arise as a consequence of decreases in oxidative phosphorylation while recognition of pathogen by neutrophils remains unaffected . Although, neutrophil related cytokines have not been formally associated with increasing levels of neutrophils, low levels of IL-8 have been observed in CFS/ME patients .
Also Check: Fatigue Muscle Weakness And Shortness Of Breath Causes
Cfs Viral Infection And Cancer
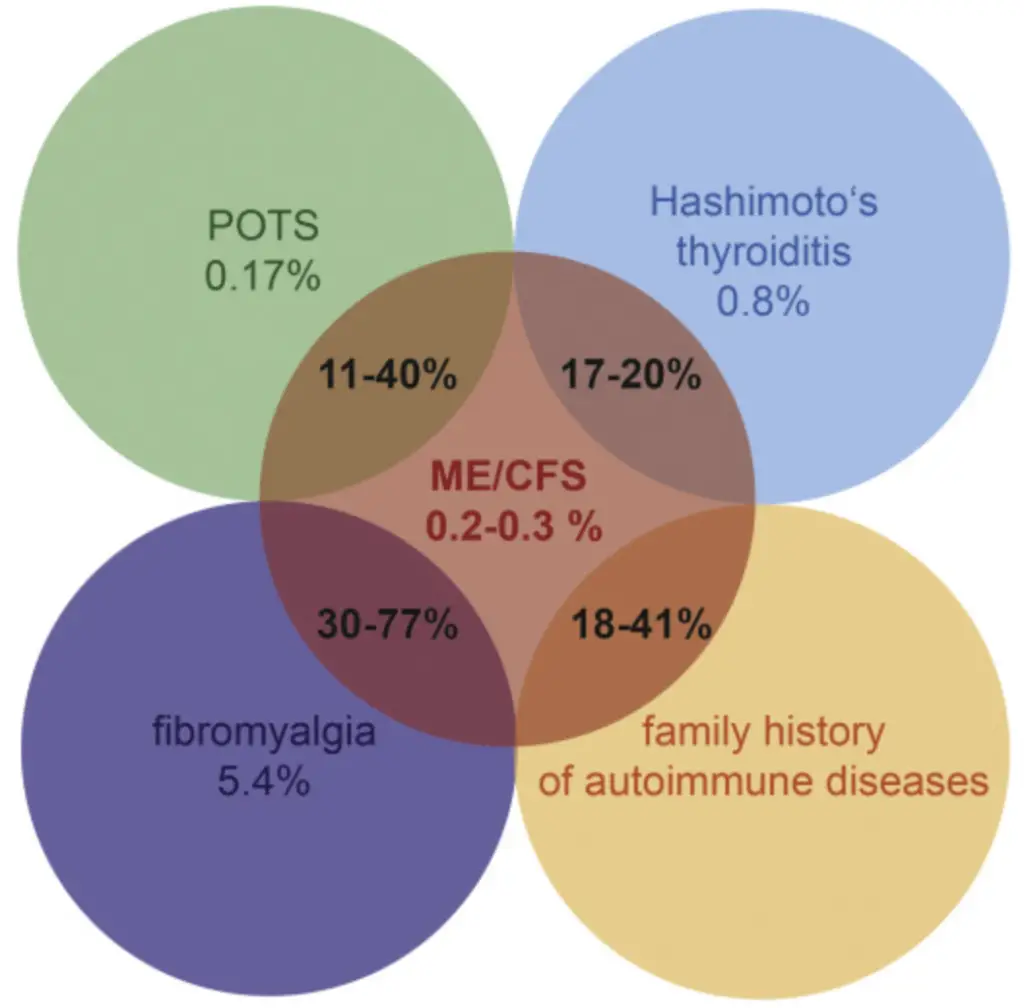
CFS is characterized by fatigue and severe disability. Besides fatigue, certain aspects of immune dysfunction appears to be present in both CFS and cancer . The underlying cause of CFS is unknown due to its heterogeneity, but in many cases, it is thought to be triggered by an abnormal immune response to an agent, such as a viral infection, that results in chronic immune activation. The immunologic changes in CFS and its possible relationship with infection have prompted investigators to consider whether CFS could also be associated with an elevated risk of cancer. A 2013 study has reported that CFS was present in 0.5% of cancer cases among US elderly and 0.5% of controls . CFS was associated with an increased risk of non-Hodgkins lymphoma and specifically NHL subtypes diffuse large B cell lymphoma, marginal zone lymphoma, and B-cell NHL not otherwise specified . In a recent clinic-based study, with a carefully selected matched cohort of 59 confirmed CFS and 54 control cases, the authors have identified statistically significant increased risks of autoimmune disease and cancer among the first-degree relatives of ME/CFS cases .
IKZF2 is highly expressed in leukemic stem cells and its deficiency results in defective LSC function. IKZF2 has been shown to drive leukemia stem cell self-renewal and inhibits myeloid differentiation. Regulation of the AML LSC program by IKZF2 thus provides a rationale to therapeutically target IKZF2 in myeloid leukemia .
Findings Show Cfs/me Is Inflammatory
Lead study author Dr. Jose Montoya and his colleagues published their findings yesterday, in the Proceedings of the National Academy of Sciences, and they suggest that that the concentration of cytokines in the bloodstream is relevant to the acuteness of CFS/ME symptoms.
The study found that variations in 17 cytokines are connected with the severity of CFS/ME in patients, suggesting that the condition is essentially an inflammatory disease.
Theres been a great deal of controversy and confusion surrounding ME/CFS even whether it is an actual disease. Our findings show clearly that its an inflammatory disease and provide a solid basis for a diagnostic blood test.
Senior author Dr. Mark Davis, Stanfords Institute for Immunity, Transplantation and Infection
Some CFS/ME patients also exhibit symptoms that are reminiscent of flu or other diseases that are associated with inflammation. Such symptoms might include a sore throat, sensitive lymph nodes, and night sweats, but also muscle pain, digestive issues, and brain fog, which is the inability to think clearly or retain focus.
Since there is no known cure for the condition, treatment normally targets the symptoms. Patients displaying signs of inflammation are often administered antivirals, anti-inflammatory drugs, or medicines that stimulate the immune system.
Recommended Reading: How To Cure Extreme Fatigue
Immune Related Proteins In Autoimmune Diseases
Cytokines and chemokines are soluble proteins with an involvement in inflammatory reactions as they can either be pro or anti-inflammatory or both. They can also be cytotoxic to certain cells and tissues. CD4+T cells are the predominant producers of both anti and pro-inflammatory cytokines. Th1 cells produce IL-2 and IFN-γ and are therefore pro-inflammatory while Th2 cells are anti-inflammatory as they produce IL-4, IL-5, IL-10 and IL-13 . The pathogenesis of most autoimmune diseases incorporates changes in these inflammatory molecules with augmented levels of these cytokines observed in the periphery and in certain tissues. For example diseases such as RA, SLE and MS are characterised by a predominant Th1 immune profile.
In CFS/ME, the cytokine profiles differ from one study to another and this may be due to other factors such as age of onset and severity or cell and tissue specific cytokines. However, it is most likely that the cytokine pattern in CFS/ME resembles that of the above described autoimmune diseases where the cytokines implicated are mainly IL-2, IL-4, IL-10, IFN-γ and TNF-α. An in-depth examination of these cytokines is necessary for establishing a definitive mechanism for CFS/ME. Governance of pro-inflammatory over anti-inflammatory or vice versa has been reported in CFS/ME and this has been observed in RA and MS hence, it is possible that in RA and MS the inflammatory status of cytokines is attributed to the diseases.
Regulatory T Cells And Autoimmune Diseases
Regulatory T cells of the immune system can be grouped in to CD8+ Tregs or CD4+Tregs. However, for the purposes of this chapter the focus will be on the CD4+Tregs which have received much attention in autoimmune diseases currently being reviewed in relation to CFS. IL-3, IL-4, IL-7, IL-15, TGF-β and CD28 are important for the development, proliferation and thrive of Treg cells . Treg profiles in a number of autoimmune disorders maybe perturbed resulting in hypo or hyperactive state in suppression. Deficiencies in Treg suppressive function may ensue from a lack in the expression of certain surface molecules such as CD39, CD95, cytotoxic T lymphocyte antigen 4 and lymphocyte activation gene 3 . Most autoimmune diseases are characterised by decreases in the function of Tregs with equivocal levels of Tregs in the tissues and periphery .
Recommended Reading: Extreme Fatigue And Body Pain
Inflammation: Helpful And Harmful
Inflammation is involved in many illnesses and injuries, and most adults have used at least one anti-inflammatory drug in their lifetime. We routinely ice and elevate our injuries to keep them from getting too inflamed.
We usually view inflammation as a problem–a symptom to be treated. However, inflammation is part of a healthy response to problems in the body. When your body detects a problemwhether it be invading viruses or bacteria, or tissues damaged from injurythe immune system triggers an inflammatory response.
What happens during an inflammatory response is that blood vessels dilate to deliver more blood to the injured area, and immune proteins are released into that blood. White blood cells flow out of the blood vessels into the problem area to kill or clean up materials that shouldnt be there. Then the tissue can begin to heal.
So when you bash your shin or twist an ankle, a little swelling is a good thing. It means the healing process is at work.
On the other hand, when inflammation becomes chronic due to ongoing damage or a misfiring immune system, then you’ve got a problem.
Ongoing damage can come from something like back pain from an injury that’s aggravated by poor posture, or repeated damage due to disease. When that damage is due to a misfiring immune system, it can mean autoimmunity.
Therapeutic Options Against Ebv: Is There A Role In Me/cfs
Limited knowledge about the origin of ME/CFS has hampered the development of effective treatment. Current strategies include administering nutritional supplements to overcome deficiencies and symptomatic treatment with analgesics, steroids or antidepressants . Thus, if a putative association between EBV infection and the onset of ME/CFS exists, the development of biomarkers that could identify patients in whom this may occur, would create a window of opportunity for tailored treatment against EBV.
Figure 2 Schematic model of treatment with DNA demethylation agents followed by adoptive immunotherapy of EBV-specific T cells. Administration of low-dose DNA demethylation agents restores the expression of MHC class II molecules and induces expression of LMP1, EBNA-2 and EBNA-3C in EBV-latency I B cells, improving the recognition of these cells by EBV-specific T cells . EBNA-1-specific CD4 T cells can only recognize latent I cells exhibiting EBNA-1 in MHC class II molecules since EBNA-1 is poorly immunogenic. DNA demethylation agents induce lytic infection and apoptosis in EBV-transformed epithelial cells. Antiviral agents prevent viral replication.
Read Also: Can Thyroid Problems Cause Fatigue
Neurovascular Unit And Vasohemodynamics
Diagram of the neurovascular unit in modulating vasohemodynamics. The neurovascular unit at the level of the cerebral microvasculature including the arterioles and capillaries is comprised of endothelial cells, smooth muscle, astrocytes, neurons, pericytes, and is modulated by surrounding microglia and perivascular macrophages. Additionally, alterations in metabolism and inflammation can modulate astrocyte end-feet to modulate cerebral blood flow . The neurovascular unit modulates blood flow throughout the brain and is regulated by energy needs of the surrounding cells and the vasoconstrictive, such as catecholamines and dopamine, and vasodilative factors, such as IL-1, TNF-, and adenosine, that are released by these cells. Pro-inflammatory molecules tend to be vasodilative, reduce vascular resistance, and increase cerebral CBF, while monoamines released by neurons have both vasodilative and vasoconstrictive properties, which can influence blood flow. Vasoconstrictive substances typically increase vascular resistance and reduce CBF.
Dont Miss: Anti Fatigue Mat For Corner Sink
When Explaining Fatigue To My Doctor What Details Are Most Important For A Diagnosis
All of the details listed are potentially important pieces of information to give your doctor, but timing, especially duration, is among the most crucial. How long has it been occurring, and has it been steady or intermittent? If the latter, how long does it last when present? Does it vary depending on the time of day? Did it start suddenly or gradually? Diagnosing the cause of fatigue can be tricky, and any assistance you can provide towards this effort will be greatly appreciated by your doctor.
As suggested in the question, another important aspect is the location of the fatigue, and whether it changes. Your doctor will also want to know if you experience more than one type of fatigue . In general, the more descriptive and inclusive you can be with your symptoms, the better chance there is of your physician being able to make a diagnosis. Still, it should be noted that a decent proportion of patients will not receive a definitive diagnosis, nor will the cause become apparent.
Finally, it is especially vital that you tell your doctor about any other symptoms or conditions, as well as any past medical history, even if you think they are entirely unrelated. In doing so, you should include any recent exposures to toxins, recent travel, medications currently taken, psychiatric issues, and complaints of snoring from others . What may appear unimportant or inconsequential to you could be an essential piece of information for your provider.
Recommended Reading: What To Do With Chronic Fatigue
Is Fatigue Classified Into Different Types By The Medical Community What Are The Most Common Types
Yes, but what they are and how many types exist depend on who you ask. It is generally accepted that fatigue can be divided into physical and mental categories, with the former involving muscles that are temporarily unable to perform optimally , while the latter describes a state of mind where cognitive function is affected negatively, such that a person is unable to think and process clearly. Mental fatigue may then be further divided into subtypes, depending on whether this is necessary for diagnosis and treatment. These should be distinguished from sleepiness caused by deprivation, although sleepiness may also be a component of non-sleep derived fatigue.
Another clinical classification system separates fatigue into three groups:
- Fatigue caused by systemic disease
- Fatigue experienced by those with neuromuscular disorders during normal exercise
- Fatigue as painful weariness, which often has no obvious cause.
In cancer patients, fatigue is categorized as either acute and related to active disease and its treatment , or, in undiagnosed patients and long-term survivors, as a more chronic form, resembling chronic fatigue syndrome . Other times, it is classified based on timing, such as with sarcoidosis, where three subdivisions are early morning, intermittent, and afternoon fatigue.
