Cdc And Webmd Collaboration
CDC partnered with WebMD to publish an informational article, titled Myalgic Encephalomyelitis/Chronic Fatigue Syndrome : The Need to Raise Awareness. Together, WebMD and CDC also produced a video that addresses the misconceptions around ME/CFS.
Links with this icon indicate that you are leaving the CDC website.
- The Centers for Disease Control and Prevention cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website’s privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance on other federal or private website.
CDC.gov Privacy Settings
We take your privacy seriously. You can review and change the way we collect information below.
These cookies allow us to count visits and traffic sources so we can measure and improve the performance of our site. They help us to know which pages are the most and least popular and see how visitors move around the site. All information these cookies collect is aggregated and therefore anonymous. If you do not allow these cookies we will not know when you have visited our site, and will not be able to monitor its performance.
Pacing Activity For People With Me/cfs
Pacing, or keeping within your available energy, is a self-management strategy to help people with ME/CFS make sure that they dont overdo activity or exercise. It reduces the likelihood of triggering PEM and can help reduce symptoms. Pacing is not a cure for ME/CFS and does not treat the underlying, physical cause of the disease.
The goal of pacing is for activity to be sustainable, so that the person can have some stability in their symptoms and what they can do each day. Pacing should be used in conjunction with rest.
The most challenging aspect of pacing is that PEM is very often delayed by as much as 24-48 hours, which can make it difficult to recognise when youve done too much. Using tools like an activity diary or heart rate monitor help you learn about your body and how much activity you can safely tolerate.
Suggestions on how to pace yourself include:
Citation Doi & Article Data
Citation:DOI:Daniel J BellRevisions:see full revision historySystems:
- Myalgic encephalomyelitis
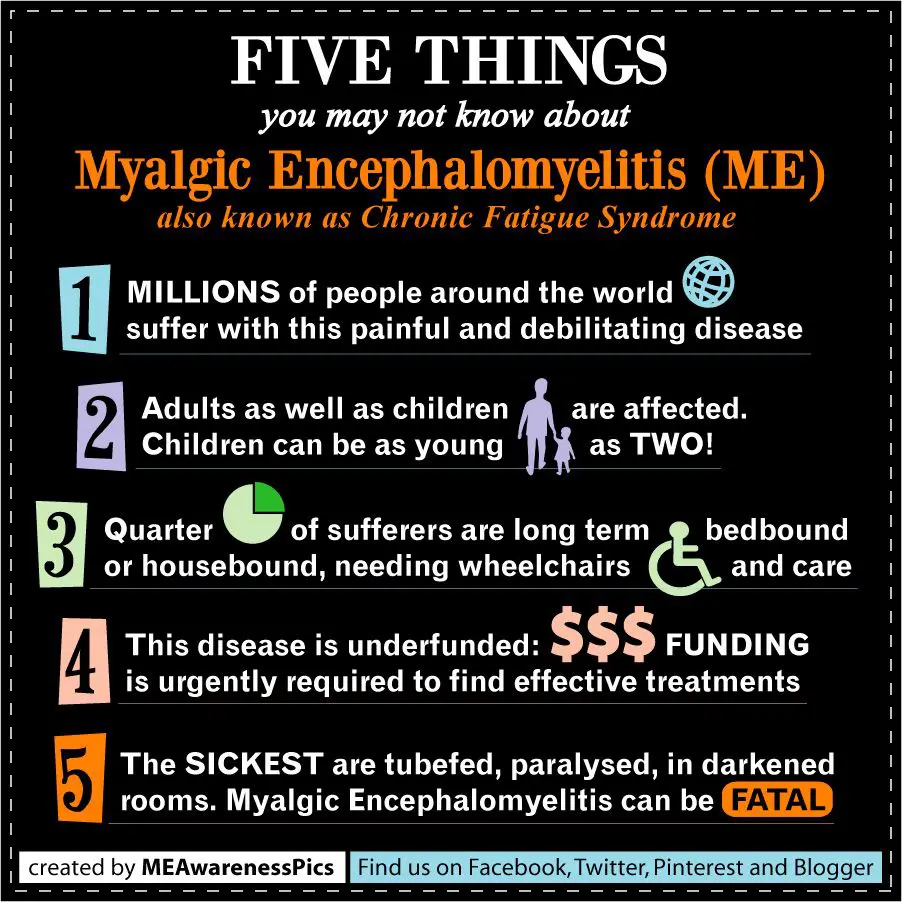
Myalgic encephalomyelitis/chronic fatigue syndrome or ME/CFS, is a complex organic disorder, characterized by profound fatigue and associated marked impairment of both physical and mental functioning. Its underlying etiology is undetermined and a curative treatment remains elusive.
Don’t Miss: Chronic Fatigue Syndrome Secondary To Ptsd
Relationship Between The School The Student The Family And The Treating Physician
During regular appointments with the young patient, the physician should ask how school is going. The clinician needs to be sensitive to the relationship between the young person, her/his parents, and the school. Many families have followed a long and circuitous route to a diagnosis and the young patient can be months or years behind in school by the time a diagnosis is reached. The young patient and parents often perceive dealing with the school to be very stressful, especially so when they face disbelief about their invisible illness from teachers, other parents, and the young patients classmates . Compounding these stresses, parents see that their childs academic performance has deteriorated and they might fear that she/he will not receive an education that eventually allows for employment and independent living. Many parents need to place their own lives and/or careers on hold in order to stay at home and take care of the young person. If both parents need to work, that can be problematic for the young patient at home alone.
How Does It Happen
Doctors don’t know what causes ME/CFS, but they have identified different underlying abnormalities in people with the condition.
Immune system problems: Several parts of the immune system are different in people with ME/CFS. Some research indicates that these abnormalities may cause the symptoms of the illness. Fortunately, people with ME/CFS don’t have a defective immune system in the way that people with HIV/AIDS do.
Energy production: In you have ME/CFS, the cells in your body have trouble making enough energy.
Brain abnormalities: Abnormalities show up in pictures of the brain , in levels of brain hormones, and in the brain’s electrical system . These abnormalities can come and go, and aren’t necessarily permanent.
Blood pressure and pulse issues: When you stand, you blood pressure could drop and your heart might start to beat faster. You might feel faint or pass out if your blood pressure drops too low.
Genes: Some studies have found abnormalities in the structure of certain genes. Others point to abnormalities in the way certain genes are turned on and off inside your cells. Studies of identical and non-identical twins indicate that some people inherit a genetic likelihood for getting the illness.
Serotonin and cortisol: Several studies indicate that serotonin, a major brain chemical, plays an important role in ME/CFS symptoms. People with the illness have low levels of cortisol, a hormone the body releases in response to stress.
Read Also: Can Pms Cause Extreme Fatigue
Physiological Findings And Physical Therapy
As most physical therapy treatments are ultimately focused on exercise and movement, physical therapists need to review the aerobic and anaerobic respiratory cycles as they relate to ME/CFS patients.
Physical therapists must recognize that research indicates the aerobic metabolism system in those with ME/CFS is broken and according to Dr. Mark Van Ness of the University of the Pacific, Classic exercise training produces little improvement and may result in PEM. He also states, Aerobic conditioning does not appear to improve or repair broken aerobic metabolism.
‘”’Dialogues for ME/CFS” is made possible with a reward from the Wellcome Public Engagement Fund. Click https://www.dialogues-mecfs.co.uk/ for access to additional scientifically-based videos on ME/CFS.”’
Pediatric Patients With Me/cfs Anticipating Surgery: Special Considerations*
Myalgic encephalomyelitis/chronic fatigue syndrome is a complex, debilitating disease characterized by severe overwhelming fatigue with a substantial loss of physical and mental functional capacity. The cardinal feature is malaise and worsening of symptoms following minimal physical or mental exertion which can persist for hours, days, or weeks and is not relieved by rest or sleep. Other symptoms include cognitive impairment, non-restorative sleep, generalized, or localized pain, and immune, neurological and/or autonomic symptoms. Remissions and relapses are common.
Most young people with ME/CFS demonstrate vasovagal syncope, postural tachycardia syndrome , neurally mediated hypotension and increased venous pooling on tilt table testing. Syncope can be precipitated by catecholamines , sympathomimetics , and vasodilators . Care should be taken to hydrate patients prior to surgery and avoid drugs that stimulate neurogenic syncope or lower BP. Many patients benefit from extra IV fluids in the perioperative period.
Propofol, midazolam, and fentanyl are generally well-tolerated. However, studies in adults have shown that some patients with ME/CFS can be sensitive to histamine-releasing anesthetic agents and muscle relaxants . If possible, they are best avoided. Young patients can also be extremely sensitive to sedative medicationsincluding benzodiazepines and antihistamines.
Garlic, gingko, and ginsengcan increase bleeding by inhibiting platelet aggregation.
Don’t Miss: Best Anti Fatigue Mat For Garage
Physiologic Responses To Upright Posture
In response to standing, approximately 500750 mL of an adults blood volume is redistributed to vessels below the level of the heart. A similar circulatory change is thought to occur in adolescents. At all ages, the response to the gravitational pooling of blood is a reduction in blood return to the heart, in turn leading to a drop in cardiac output, less stretch of baroreceptors, and ultimately less blood flow to the brain. The nervous system response involves an increase in sympathetic neural outflow, improved vasoconstriction, up to a 40 bpm increase in HR, and the return of enough venous blood to maintain BP and cerebral perfusion . Symptoms of OI can appear when these adjustments do not occur in an efficient manner.
Figure A1. The three main pathophysiologic influences on orthostatic intolerance are shown in this Figure. Increased pooling of blood, or defective vasoconstriction in the lower half of the body, along with lower intravascular volume are each important, and can be present in the same individual. Upon assumption of an upright posture, exaggerated sympathetic nervous system and adrenal hormone responses lead to increased release of epinephrine and norepinephrine . It is postulated that the relative balance of NE to Epi is one factor in determining whether the phenotype of OI is POTS or neurally mediated hypotension . Some patients with POTS in the early phase of orthostatic testing go on to develop a classic NMH pattern later in the test.
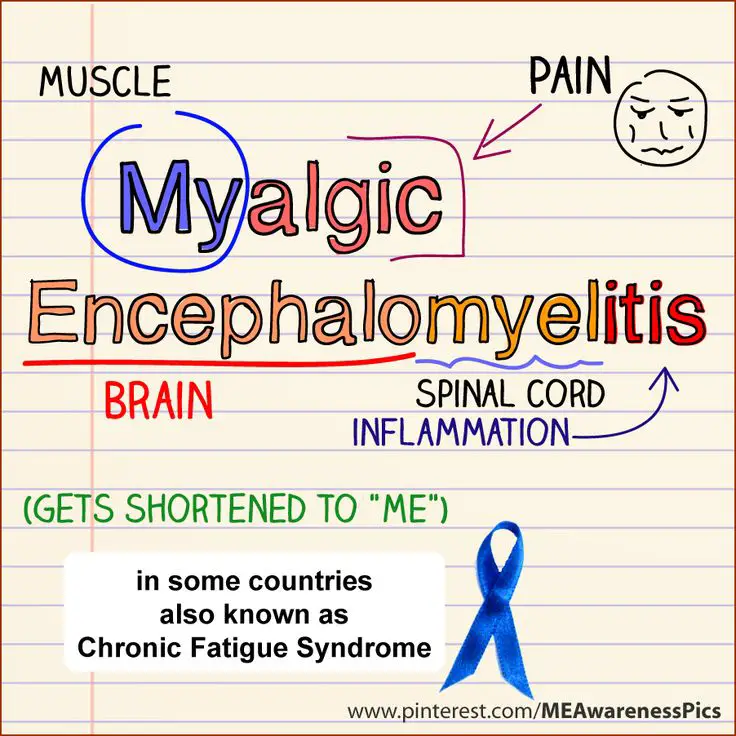
Why Use Myalgic Encephalomyelitis
Several countries around the world currently use the term myalgic encephalomyelitis instead of chronic fatigue syndrome, both for research purposes and when diagnosing the illness. This term appears to be gaining traction in the United States among researchers, advocates, and people with the disease, as well. Some people use the terms interchangeably, while others consider them separate conditions.
Patients, advocates, and some researchers in the U.S. have pushed for the use of ME/CFS due to the widespread belief that the name “chronic fatigue syndrome” trivializes the condition and leads to misconceptions about it. Once the public and medical community are better acquainted with the term, they plan to drop the “CFS” portion altogether and just use ME as the condition’s name.
However, a major report from the Institute of Medicine has called for the name of this condition to be changed to systemic exertion intolerance disease, abbreviated as SEID. That’s based on the widespread abnormalities associated with the illness and, especially, one of its distinguishing symptomspost-exertional malaise . PEM is an extreme negative reaction to exertion and an inability to repeat the same level of activity the following day.
It remains to be seen whether the name SEID will find acceptance. It faces an uphill battle since many researchers have transitioned to myalgic encephalomyelitis/chronic fatigue syndrome in their published papers.
Recommended Reading: Fatigue After Radiation Therapy Breast Cancer
Alternative And Complementary Medicine
Many alternative and complementary therapies have been promoted for ME/CFS. It is difficult to determine whether these therapies actually work, because the symptoms of ME/CFS vary so much from day-to-day. Anecdotal evidence suggests that acupuncture, massage, pilates, and yoga can help pain in some adults, but no published studies have assessed their benefit in young people.
The clinician should identify the use of herbal/natural remedies or supplements. The contents of complementary medicines are not regulated for dose or composition. Caution must be exercised regarding side effects because if used with prescribed medications, there can be interactions.
Unfortunately, in the hope of a cure, parents of young patients with ME/CFS often ask the young patient to try costly, non-established and speculative treatments but find little or no clinical improvement. Feedback from young people with ME/CFS indicated that 80% had tried up to 30 different alternative therapies. Only massage for pain relief and good dietary advice achieved some benefit in up to 30% of patients. A common comment from the patients was that they were glad when their parents stopped shopping around for a cure. . A review of alternative medicine studies in adults with ME/CFS revealed generally poor methodologies and limited evidence of any benefit .
How Is Me/cfs Treated
There is currently no FDA-approved treatment or drug for ME/CFS. As neither a cause nor cure for ME/CFS has been identified, treatment is directed at relieving symptoms. However, there are interventions and symptom-reduction strategies that you can use to significantly improve patients quality of life.
Learn more in our Patient Resources section.
Studies show that less than 9-16 percent of ME/CFS patients in the United States have been properly diagnosed. Diagnosing ME/CFS is a challenging process because there is still not one diagnostic test or biomarker thats conclusive. Getting a definitive diagnosis often takes months or even years.
Providing compassionate and effective care for patients with ME/CFS can be challenging, like many other multisystemic chronic conditions. Patients and their providers must be partners with open lines of communication in order to effectively manage this illness. For medical providers seeking to provide better care for ME/CFS patients, reference our educational materials at our Medical Provider Resources page.
Recommended Reading: Medications For Chronic Fatigue Syndrome
Symptom Management For People With Me/cfs
Refer to relevant NICE guidance for managing symptoms that are not covered in this section, taking into account the recommendations in the , and .
Rest and sleep
-
- about the role of rest in ME/CFS
- that rest periods are part of all management strategies for ME/CFS
- how to introduce rest periods into their daily routine, including how often and for how long, as appropriate for each person
- that relaxation techniques at the beginning of each rest period could be helpful.
- 1.12.2.
-
Give people with ME/CFS personalised sleep management advice that includes:
- explaining the role and effect of sleep disturbance in ME/CFS
- identifying the common changes in sleep patterns seen in ME/CFS
- developing good sleep habits
- taking into account the need for rest in the day, and balancing this against how the person is sleeping at night
- introducing changes to sleep patterns gradually.
- 1.12.3.
-
If sleep management strategies do not improve the persons sleep and rest, think about the possibility of an underlying sleep disorder or dysfunction and whether to refer to an appropriate specialist.
- 1.12.4.
-
Review the use of rest periods and sleep management strategies regularly as part of the persons .
For a short explanation of why the committee made these recommendations and how they might affect practice, see the .
Full details of the evidence and the committees discussion are in evidence review G: non-pharmacological management of ME/CFS.
Physical functioning and mobility
Orthostatic intolerance
Pain
Lack Of Knowledge About Me/cfs Dysautonomia Hampering Patient Care
In research surrounding long COVID, one term that comes up a lot is ME/CFS. This multisystem illness usually appears after a viral or bacterial infection, and is characterized by severe fatigue that causes a substantial reduction in their ability to participate in daily social and occupational activities, as well as a huge increase in negative symptoms directly following exercise, called postexertional malaise.
The fatigue experienced by those with ME/CFS can be extreme most patients are unable to work, according to the review.
Many researchers have commented on the similarity between ME/CFS and long COVID around half of individuals with long COVID are estimated to meet the criteria for ME/CFS, and in studies where the cardinal ME/CFS symptom of postexertional malaise is measured, a majority of individuals with long COVID report experiencing postexertional malaise, the authors wrote.
Another issuing surfacing in long COVID patients is dysautonomia, which is frequently comorbid with ME/CFS, particularly a type of dysautonomia called POTS, in which a person heart rate abnormally spikes after sitting up or standing.
This figure shows some of the theories behind long COVID pathogenesis, including immune dysregulation, microbiota disruption, autoimmunity, clotting and endothelial abnormality.
Dysautonomia is also often misdiagnosed as psychiatric or psychological disorders due to its symptoms presenting as similar to mental health issues such as anxiety.
Don’t Miss: Global Industrial Anti Fatigue Mats
Box 5cognitive Behavioural Therapy
The committee wanted to highlight that cognitive behavioural therapy has sometimes been assumed to be a cure for ME/CFS. However, it should only be offered to support people who live with ME/CFS to manage their symptoms, improve their functioning and reduce the distress associated with having a chronic illness.
For a short explanation of why the committee made these recommendations and how they might affect practice, see the .
Full details of the evidence and the committees discussion are in evidence review G: non-pharmacological management of ME/CFS and appendix 2: involving adults with severe ME/CFS.
Who Is It For
- Health and social care professionals, including those working or providing input into educational and occupational health services
- People with suspected or diagnosed ME/CFS, their families and carers and the public
This guideline was commissioned by NICE and developed at the National Guideline Centre which is hosted by the Royal College of Physicians.
This guideline updates and replaces NICE guideline CG53 .
Read Also: What Can Cause Leg Fatigue
Children Young People And Me/cfs
ME/CFS can affect people of all ages, including the very young. Young people with ME/CFS, especially children under the age of ten, might have trouble knowing or articulating that something is wrong. They may not realise that their loss of stamina, or other symptoms they are experiencing, are not normal. Alternatively, they may not have the words to describe what they are feeling.
For both younger children and teenagers, schooling can be affected but ME/CFS is not school refusal. While school refusal can often be accompanied by physical complaints , and these complaints may tend to disappear when the young person stays home, the pattern is different with ME/CFS. In a young person with ME/CFS, some symptoms never ease and symptom exacerbation is triggered by activity. In ME/CFS, symptoms are likely to be worse after school attendance, and can reduce with pacing and rest, which includes time away from school or during holidays.
Some young people with ME/CFS can continue to attend school, and others may be too unwell for regular classroom attendance. Parents, healthcare providers, schools and the child or teenager need to work together to come up with a plan for the young persons continued education. This plan needs to take into account the energy limits of ME/CFS. Being creative and flexible is key and might include things like fewer subjects or school from home.
Housebound Or Bedbound With Me/cfs
About 25% of people with ME/CFS are housebound or bedbound. Those who are housebound may be able to undertake minimal daily tasks for themselves, such as brushing teeth, cooking or using a computer for short periods of time, but they have to pace their activity and often use aids to help them . They are unable to leave the house, often because this requires more energy than they have available. When they do leave the house, they often need mobility aids such as a wheelchair or mobility scooter, or other assistance . Recovery from a trip out of the house can take days, or longer.
Some people are so severely unwell that they are bedbound some or all of the time. The most severely unwell may be unable to undertake even simple tasks, like eating or going to the toilet by themselves. They may require additional medical devices, such as feeding tubes, to help them get enough nutrition and fluids, and can be totally dependent on carers.
You May Like: Do Allergies Cause Fatigue And Body Aches