How Long Does Covid Last
Mild or moderate COVID-19 lasts about two weeks for most people. But others experience lingering health problems even after the fever and cough go away and they are no longer testing positive for the illness.
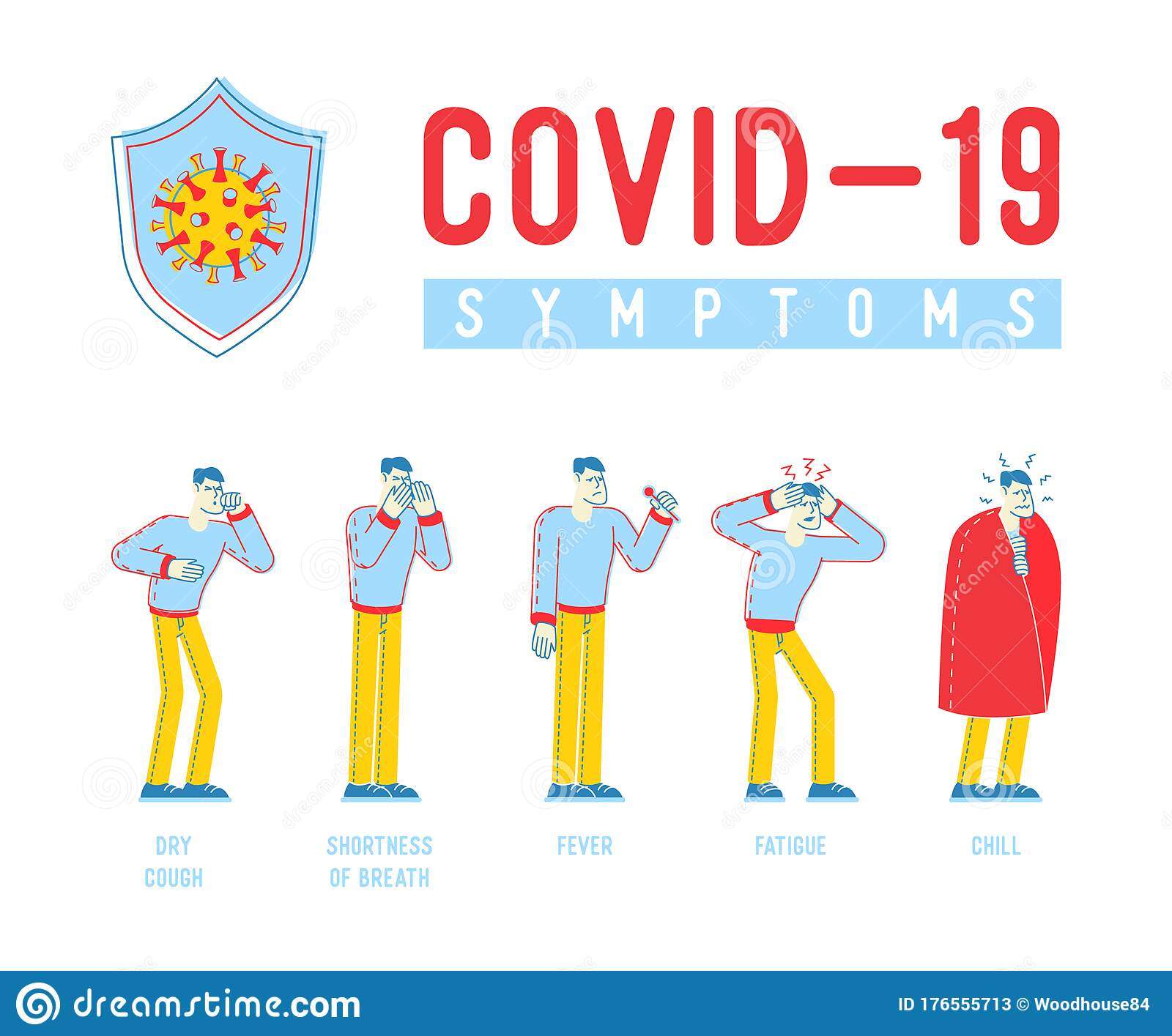
Parker notes that the World Health Organization has developed a definition for post-COVID-19 condition as coronavirus symptoms that persist or return three months after a person becomes ill from infection with SARS CoV-2, the coronavirus that causes COVID-19. Those symptoms can include:
- Shortness of breath
- Cognitive problems
The symptoms can come and go, but have an impact on the persons everyday functioning, and cannot be explained by another health problem.
Whats The Difference Between A Dry Cough And A Wet Cough
A cough is your bodys way of clearing the lungs and airways of irritants so you can breathe better.
When you have an illness that affects your respiratory system, you may cough up mucus. This is a wet cough. Healthcare providers consider a wet cough to be productive because it clears phlegm from the lungs and airways. If too much phlegm builds up in the lungs, you may become short of breath and develop other problems.
When you have a dry cough, nothing comes up. This unproductive cough doesnt open up the lungs or air passages.
How Can I Protect My Child
- Washing your hands and your childs hands is the best thing that you can do to stop the spread of germs. Wash your hands after:
- Coughing or sneezing into your hands or wiping your nose.
- Using the toilet or helping your child to use the toilet
- Caring for someone with any kind of infection.
- Cleaning up vomit or diarrhea.
- Wiping your childs nose.
- Handling raw meat.
- Handling pets or animals.
Read Also: The Fatigue Short-sleeve Jumpsuit
Causes Of Glandular Fever
Glandular fever is caused by the Epstein-Barr virus . This virus is found in the saliva of infected people and can be spread through:
- kissing glandular fever is often called the kissing disease
- exposure to coughs and sneezes
- sharing eating and drinking utensils, such as cups, glasses and unwashed cutlery
If you have EBV, its a good idea to take steps to avoid infecting others while you are ill, such as not kissing other people.
Formation Of Subgroups With Excessive Daytime Sleepiness And Severe Fatigue
There is only a slight connection between excessive daytime sleepiness and fatigue thus, a prediction of excessive daytime sleepiness from fatigue and vice versa is not possible. It is, therefore, useful to study excessive daytime sleepiness and fatigue as independent factors.
Four patient groups were formed to estimate the risks for excessive daytime sleepiness and severe fatigue. Group 1 consisted of 878 patients in whom neither fatigue nor daytime sleepiness showed excessive levels. Group 2 consisted of 122 patients with excessive daytime sleepiness, and group 3 included 123 patients with severe fatigue. Seventy-four patients of group 4 were characterized as having both severe fatigue and excessive daytime sleepiness. A ranking of the 4 groups cannot be performed therefore, 3 binary prediction models for excessive daytime sleepiness and severe fatigue were developed individually and in combination.
Also Check: Extreme Fatigue And Aching Joints
Heart Problems In Covid Long Haulers
SARS-CoV-2 infection can leave some people with heart problems, including inflammation of the heart muscle. In fact, one study showed that 60% of people who recovered from COVID-19 had signs of ongoing heart inflammation, which could lead to the common symptoms of shortness of breath, palpitations and rapid heartbeat. This inflammation appeared even in those who had had a mild case of COVID-19 and who had no medical issues before they got sick.
Food Tastes Like Metal
Why this happens:
A build-up of wastes in the blood can make food taste different and cause bad breath. You may also notice that you stop liking to eat meat, or that you are losing weight because you just dont feel like eating.
What patients said:
Foul taste in your mouth. Almost like youre drinking iron.
I dont have the appetite I had before I started dialysis, I must have lost about 10 pounds.
Also Check: How To Combat Fibromyalgia Fatigue
You May Like: What Is The Best Supplement For Adrenal Fatigue
Do Covid Vaccines Prevent Long Covid
Getting vaccinated for COVID-19 lowers the risks of COVID infection. While breakthrough infections are possible, being fully vaccinated and boosted is effective in reducing the risk of hospitalization and death due to COVID. Research is ongoing about how long COVID affects people who had breakthrough COVID, but it is likely that being vaccinated reduces the risk.
Shortness Of Breath Jaw Pain Fatigue: 3 Common Symptoms That Women Shouldnt Ignore
Between working, childcare, and yes, even scheduling doctors appointments for spouses and parents, that fatigue or pesky jaw pain is simply brushed off by many women.
And while many symptoms may be nothing more than a passing discomfort, there are other times when it may be a sign that there is something more serious going on.
Its important for women to understand that theres no duration of a symptom that automatically makes it a red flag other than crushing chest pain, some things can wait, said NBC News medical contributor Dr. Natalie Azar. There are also very benign explanations for a lot of things as well as more serious explanations.
Whats important is to first, be aware of what youre feeling and take note of whats normal for your body, and second, seek answers from your healthcare provider when something does feel off.
Here are three symptoms that women shouldnt ignore:
You May Like: Sore Throat And Chronic Fatigue
Acute Vs Chronic Bronchitis
Acute bronchitis most often develops after youve had a viral or bacterial infection. But, other irritants, such as smoke, dust, or fumes, can also cause acute bronchitis. Acute bronchitis symptoms usually subside after 7 to 10 days, but you might still cough for several weeks.
Chronic bronchitis happens when you have repeated attacks of bronchitis. Its defined as having a productive cough that lasts at least three months, with recurring episodes for at least two straight years. Smoking causes more than 80 percent of all cases of chronic bronchitis.
Sometimes, people who have frequent episodes of acute bronchitis go on to develop chronic bronchitis.
People At Higher Risk From Flu
Anyone can get sick with flu, even healthy people, and serious problems related to flu can happen to anyone at any age, but some people are at higher risk of developing serious flu-related complications if they get sick. This includes people 65 years and older, people of any age with certain chronic medical conditions , pregnant people and children younger than 5 years, but especially those younger than 2 years old.
Don’t Miss: Constant Brain Fog And Fatigue
Should I Be Worried About My Dry Cough
Its normal to cough when something tickles your throat or a piece of food goes down the wrong pipe. After all, coughing is your bodys way of clearing your throat and airways of mucus, fluids, irritants, or microbes. A dry cough, a cough that doesnt help to expel any of these, is less common.
A dry, hacking cough can be irritating. But it could also be a sign of something more serious, such as chronic lung disease. If youve got a persistent dry cough, here are a few reasons why you should get it checked out by a doctor.
Dont Miss: How To Get Out Of Adrenal Fatigue
What Other Symptoms Might I Have

If your breathing problems are caused by a cold or chest infection, you might also have a cough, fever, sore throat, sneezing, blocked or runny nose and general congestion.
If the problem is to do with your heart, you might also have chest pain, feel light-headed and nauseous. If you have been diagnosed with angina, take your medication as directed. Wait 5 minutes and take another dose.
If the problem is asthma or chronic obstructive pulmonary disease , you might also have a lot of mucous, a wheezing sound when you breathe, and your symptoms might get worse with exercise or during the night.
If the problem is a panic attack, you might also have a fast heartbeat, sweating and shaking, nausea, dizziness and a sense of impending doom or danger.
Read Also: Stomach Pain Loss Of Appetite Nausea Fatigue
Long Covid Symptoms In Children And Teens
Its not yet known whether children who have had COVID-19 are more or less likely than adults to experience continuing symptoms. But long-term COVID-19 in children is a possibility, showing up as fatigue, headaches, difficulty with school work, mood concerns, shortness of breath and other long-hauler symptoms.
Amanda Morrow, M.D., a specialist in physical medicine and rehabilitation, is part of the multidisciplinary team at Kennedy Krieger Institutes Pediatric Post COVID-19 Rehabilitation Clinic, which addresses lingering coronavirus symptoms in children and teens. She says it isn’t clear why long COVID-19 symptoms affect some children and not others.
We are seeing patients who are often very high-functioning, healthy children who did not have any previous illnesses or medical conditions, she says, noting that many of the kids being treated at the clinic only had mild bouts of COVID-19.
Heart inflammation after COVID-19 is a concern, especially among young athletes returning to their sports after a mild or even asymptomatic case of the coronavirus. They should be screened for any signs of heart damage to ensure it is safe for them to resume activity.
Kids who have experienced the uncommon but serious complication of COVID-19 called multisystem inflammatory syndrome in children, or MIS-C, can be left with serious heart damage, and should be followed by a pediatric cardiologist.
More Information Will Emerge On Long
SARS-CoV-2, the virus that causes COVID-19, was identified in December 2019. There is still a lot to learn about it, but our understanding of the virus and COVID-19 is evolving by the day.
Researchers will learn more about how and why the coronavirus affects different people in such a variety of ways, and why some people experience no symptoms at all while others have life-threatening organ damage or lasting disability. New insights will provide avenues for therapies and hope for people living with long-term COVID-19 effects.
Recommended Reading: Mega Comfort Anti Fatigue Mat Esd
Safety First A Checklist Of Warning Signs Of More Serious Breathing Problems
Its nice that some people may be able to find an easy solution to their shortness of breath, or at least be reassured that its mostly harmless. Unfortunately, more ominous causes of dyspnea are also common, so please always alert your doctor about any difficult breathing. If your doctor cannot find any explanation, and you have none of these red flags, then you can pursue the possibility of muscle knots and weak breathing muscles. Safety first! And second.
- Have you developed other unusual and/or persistent symptoms?
- Do you have a chronic wheeze or cough?
- Are you tired all the time? Do you look pale? These two together are a red flag.
- Do you have a dry, painful cough and your shortness of breath gets worse when you exercise?
- Are your feet and ankles swollen, and is it harder to breathe when you lie down flat?
- Have you worked in or around asbestos, wood dust, industrial fumes or in a coal mine? If so, you probably already understand why youre having trouble!
Any of these factors could be associated with a slow, sneaky onset of a serious condition.
The Timing Of Symptoms Matters
While the symptoms themselves may overlap a bit, the timing of those symptoms may help you determine what illness your child has. This is called the incubation period or how long it takes symptoms to appear after exposure.
Though incubation periods can vary, they are roughly:
- 24 to 72 hours for a cold
- 1 to 4 days for influenza
- 2 to 14 days for COVID-19, with an average of 5 days
When possible, try to monitor who your child interacts with and when. By identifying the most recent time your child may have been exposed, you may be able to use that information to help determine which illness your child is experiencing.
Recommended Reading: Dizzy Shortness Of Breath Fatigue
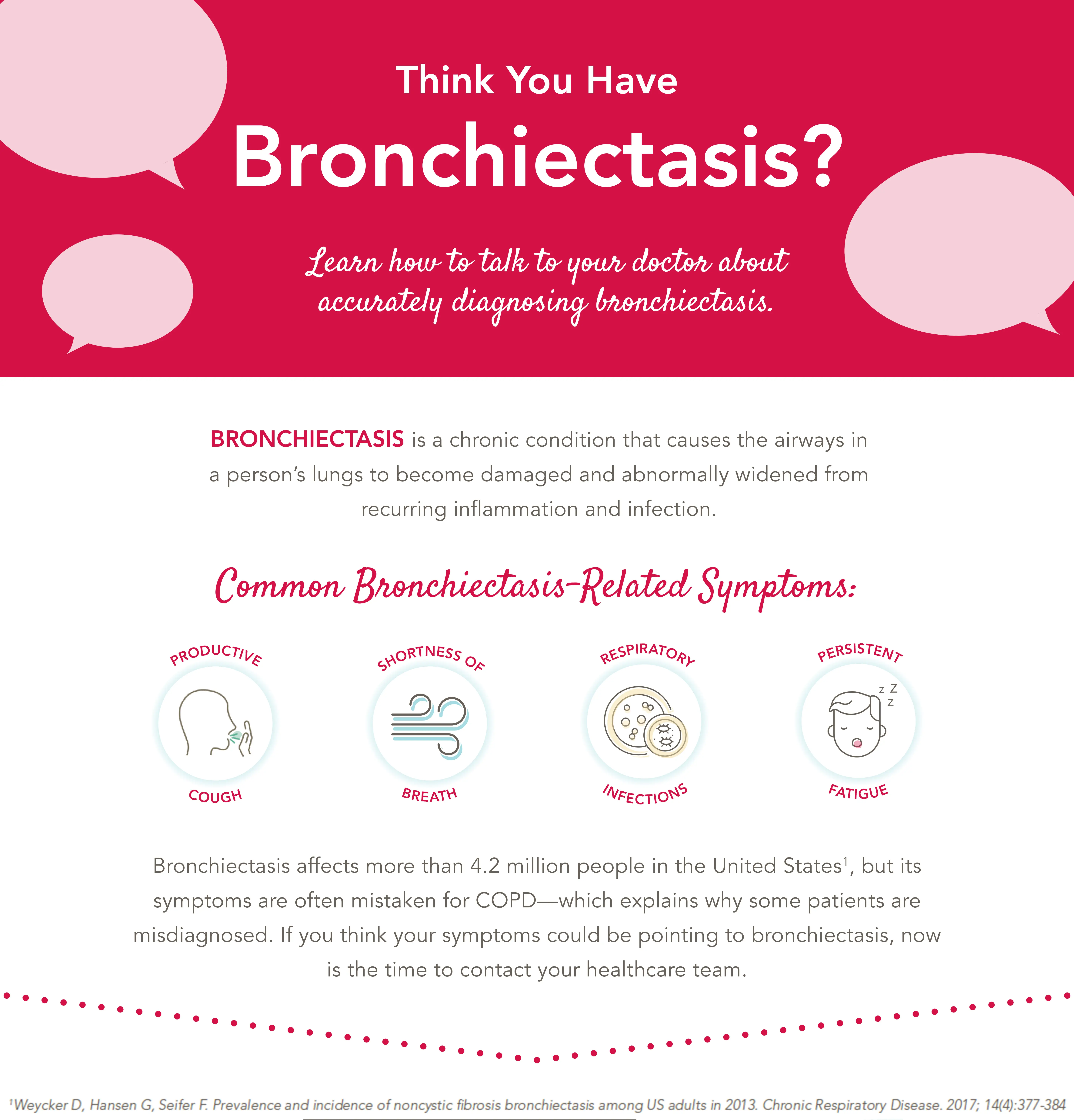
Shortness Of Breath With Nonproductive Cough And Fatigue
Vol. 12 Issue 3 Page 21Shortness of Breath With Nonproductive Cough and Fatigue
A 24-year-old African-American woman presented to the fast-track emergency department three times with subjective complaints of shortness of breath. She was evaluated by three different nurse practitioners. She reported taking no routine medications.
On her initial visit, her chief complaint was shortness of breath and a nonproductive cough for 1 day. Her physical examination was unremarkable. Her lungs were clear, pulse rate 80, respiratory rate 16, temperature 98 degrees and blood pressure 146/79 mmHg her oxygen saturation was 100%. She reported no previous medical problems. She was diagnosed with an upper-respiratory infection, and the NP prescribed over-the-counter cold medicines.
Two weeks later, she reported continued subjective complaints of shortness of breath and nonproductive cough, as well as new onset dyspnea on exertion. Her physical examination was again unremarkable. Her lungs were clear, pulse rate 72, respiratory rate 16, temperature 98.7 degrees and blood pressure 132/76 mmHg her oxygen saturation was 98%. The NP diagnosed bronchitis and prescribed Tessalon Perles for cough, vitamin C 500 mg twice a day and increased fluid intake.
Differential Diagnosis
Diagnostic Testing
Discussion
Remember the saying: If you hear hoof beats, do you think of horses or zebras? Sometimes its a zebra.
References
Read Also: Vitamin D Deficiency And Fatigue
A Quick Success Story About Sore Breathing Muscles
I once developed a sharp pain in the side of my neck when I coughed or sneezed. It was clearly a muscular pain,12 specifically of the scalenes muscle group that kick in when you breathe hard. If I took a really deep breath, I could feel it a little too but it was mostly only clear when I coughed or sneezed.
Until I went for a run.
After a few minutes of huffing and puffing, that pain started up. I also felt distinctly short of breath, despite being generally quite fit. The pain was like a stitch in my side, but in my neck, and I was not getting full breaths. I realized I was barely using my diaphragm to breathe, and so my scalenes were working overtime to make up the difference and hurting and failing. I started using my diaphragm again and the pain steadily eased even though I kept running.
Not only was the pain clearly caused by over-using my scalenes while breathing, but I was able to fix a fairly significant pain problem without stopping my workout just by breathing differently. Thats a good, clear example of the easiest kind of breathing trouble to fix. What was going on?
Read Also: High Blood Pressure Nausea Fatigue
Shortness Of Breath: When To See Your Doctor
Sep 30, 2019Cara Martinez
Shortness of breath can be brought on by many thingssome more serious than others.
Causes can include aerobic exercise, intense physical activity, asthma, anxiety, or being in high altitude. And in some cases, shortness of breath can be the symptom of a lesser-known life-threatening condition.
When searching for an undetected cause of shortness of breath, we first look to the heart, lungs, and circulatory system. Then, we look for 5 signs that will guide us toward the right diagnosis.
Here, Cedars-Sinai experts explain some of the conditions responsible for shortness of breath and when you should see your doctor.
Why Should You Care
Even survivors with mild initial symptoms can have persistent symptoms that last for a month or more after infection with COVID-19.
Top 5 Symptoms of Long COVID
If you are experiencing lingering symptoms after being infected with COVID, or you feel worse or develop any new symptoms, you should contact your healthcare provider. The American Lung Association has also launched a Long COVID online community to offer additional support.
You May Like: What Can Cause Sudden Extreme Fatigue
Despite Recovering From Covid
Advanced testing of the heart and lungs may reveal why some people who have recovered from COVID-19 still have shortness of breath. This testing is highly specialized and available only at a few sites nationwide, including at Yale.
Many patients continue to have ongoing symptoms well after their initial SARS-CoV-2 infection. Symptoms are not limited to those who required hospitalization or ICU admission and commonly occur in those with a history of mild COVID-19. Patients often have normal findings on tests such as lung function testing, chest X rays or CT scans. Physicians at the Winchester Center for Lung Disease have been exploring additional ways to evaluate patients with post-COVID-19 conditions, who are also known as Long Haulers.
Singh and colleagues, including PVDP Associate Director Phillip Joseph, MD, recently published original research in CHEST Journal in which they discussed how patients who have recovered from mild cases of COVID-19 without cardiopulmonary disease have a marked reduction in their peak oxygen consumption. Singh said this is because of impaired oxygen extraction by the muscles.
The team is planning more studies. Were drawing blood when the patients are at rest and at the peak of exercise to see if theres any circulating biomarker that could explain our findings, said Singh.